10.20986/revesppod.2025.1712/2024
REVIEW
Use of elastography in podiatry: a bibliographic and systematic review of evidence in the diagnosis and management of foot problems
Uso de la elastografía en podología: revisión sistemática de evidencias en el diagnóstico y manejo de patologías del pie
Ana M.ª Rayo Pérez1
Rafael Rayo Martín1
Francisco Javier Rodríguez Castillo1
Raquel García de la Peña1
1Departamento de Podología. Universidad de Sevilla, España
Abstract
Objectives: Elastography has emerged as a non-invasive diagnostic tool for assessing the stiffness and elasticity of tissues, with potential applications in the field of podiatry for the detection and management of various pathologies, such as plantar fasciitis and tendinopathies. To evaluate the available evidence regarding the use of elastography in podiatry for the diagnosis, management, and follow-up of foot pathologies.
Material and methods: A systematic review and meta-analysis were conducted following the PRISMA guidelines, including studies that assessed the effectiveness of elastography in podiatric conditions, utilizing databases such as PubMed, Scopus, and Cochrane, and applying predefined inclusion and exclusion criteria to ensure the quality and relevance of the studies.
Results: Eight articles of high methodological quality and low risk of bias were included, consistently demonstrating the utility of elastography in evaluating various podiatric pathologies, with elevated sensitivity and specificity in detecting changes in tissue elasticity, particularly in conditions such as plantar fasciitis and tendinopathies.
Conclusion: The systematic review and meta-analysis conducted on the use of elastography in podiatry indicate that several interventions, including eccentric and isometric exercises, extracorporeal shock wave therapy (ESWT), and radiofrequency treatment, have a positive impact on reducing tendon stiffness and improving functionality.
Keywords: Elastography, podiatry, tendinopathy, plantar fasciitis, ultrasound
Resumen
Objetivos: La elastografía ha emergido como una herramienta diagnóstica no invasiva para evaluar la rigidez y elasticidad de los tejidos, con aplicaciones potenciales en el campo de la podología para la detección y manejo de diversas patologías, como la fascitis plantar y las tendinopatías. Evaluar la evidencia disponible sobre el uso de la elastografía en podología para el diagnóstico, manejo y seguimiento de patologías del pie.
Material y métodos: Se realizó una revisión sistemática y metanálisis siguiendo las directrices PRISMA 2020. Se incluyeron estudios que evaluaron la efectividad de la elastografía en patologías podológicas, utilizando bases de datos como PubMed, Scopus y Cochrane. Se aplicaron criterios de inclusión y exclusión predefinidos para asegurar la calidad y relevancia de los estudios. La selección de estudios, extracción de datos y evaluación del riesgo de sesgo fueron realizadas por 2 revisores independientes.
Resultados: Se incluyeron 8 artículos de alta calidad metodológica y bajo riesgo de sesgo. Los resultados demostraron consistentemente la utilidad de la elastografía en la evaluación de diversas patologías podológicas, con una sensibilidad y especificidad elevadas en la detección de cambios en la elasticidad tisular, particularmente en condiciones como la fascitis plantar y las tendinopatías.
Conclusión: La elastografía es una herramienta útil para el diagnóstico y seguimiento de patologías del pie, con un impacto positivo en la reducción de la rigidez tendinosa y la mejora de la funcionalidad. Sin embargo, se requiere más investigación para estandarizar su uso y evaluar su eficacia en diversas condiciones podológicas.
Palabras clave: Elastografía, podología, tendinopatía, fascitis plantar, ecografía
Corresponding author
Ana M.ª Rayo Pérez
anarayo43@gmail.com
Received: 09-10-2024
Accepted: 24-02-2025
Introduction
Elastography is an imaging technique used to analyze the mechanical properties of tissues, especially their elasticity and stiffness. This methodology is based on assessing the tissue response to an external force, either through manual compression or ultrasound. Elastography allows the acquisition of elasticity maps that provide useful data about the health status of tissue, facilitating the detection and characterization of various diseases(1,2,3).
One of the most notable uses of elastography is its ability to identify changes in tissue stiffness, which may indicate the presence of pathological processes such as inflammation, fibrosis, or tumors. Clinically, elastography has proven particularly beneficial for evaluating liver diseases, musculoskeletal injuries, and, more recently, in the field of podiatry. In this area, the method is used for the diagnosis and follow-up of several conditions affecting the foot and ankle, including plantar fasciitis, tendinopathies, and overuse injuries(2,4,5).
One of elastography’s greatest strengths is its non-invasive nature, which allows repeated assessments without causing harm to the patient. This is especially relevant in podiatry, where patients may have chronic diseases that require ongoing monitoring. Additionally, elastography provides numerical data on tissue elasticity, which can be more objective and reproducible compared to conventional clinical assessments that often rely on the examiner’s experience(6,7).
Elastography also facilitates the differentiation of various tissue types, offering insights into tissue composition. This can be critical for identifying lesions that might not be visible on traditional ultrasound, such as small tendon tears or degenerative changes in ligamentous structures. This ability to detect subtle changes in tissue elasticity may aid in the early diagnosis of diseases, thereby improving treatment and recovery outcomes(3,4,8)
However, despite its numerous benefits, elastography also has limitations. One of the main challenges lies in the variability of image acquisition and analysis methods, which can lead to inconsistent results. Moreover, interpreting elastographic data requires specific training and clinical experience, which may limit its use in settings where such resources are unavailable. It is also essential to consider that elastography may not be suitable for all patients, particularly those with conditions that impair their ability to remain still during the evaluation(9,10).
In podiatry, the use of elastography offers a novel and promising method for diagnosing and treating various foot conditions. As research continues to explore its effectiveness and utility, it is anticipated that this method will become more integrated into routine clinical practice, providing healthcare professionals with more precise tools for assessing and managing foot disorders. As elastography advances, its integration with other imaging and clinical assessment modalities could further enhance the understanding of podiatric conditions and improve treatment plans for patients(5,11,12).
Therefore, the main objective of this article is to evaluate the available evidence on the use of elastography in podiatry for the diagnosis, management, and follow-up of foot disorders. Additionally, the aim is to determine the reliability and validity of elastography in the assessment of common podiatric conditions (plantar fasciitis, tendinitis, among others).
Material and methods
This is a systematic review that follows the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
Sample
Inclusión criteria were studies of patients of any age and sex with diagnosed or suspected podiatric conditions, use of elastography in any of its modalities (shear wave elastography, strain or compression elastography) and clinical trials, observational studies (cohort, case-control, cross-sectional), previous systematic reviews, and technology assessment studies.
Exclusion criteria were studies not specifically evaluating the use of elastography in podiatric conditions, case reports or case series without a comparison group and studies without full-text access or not available in English or Spanish.
Information sources and search strategy
Comprehensive searches were conducted across these databases: PubMed, Scopus, Web of Science, and Cochrane Library. References from relevant studies were also reviewed to identify other potentially eligible studies. No time limit was applied, but the search focused on recent studies (last 10 years).
The following combinations of MeSH terms and keywords were used:
- “Elastography” OR “Elastografía”.
- “Podiatry” OR “Podología”.
- “Plantar fasciitis” OR “Fascitis plantar”.
- “Tendinopathy” OR “Tendinopatías”.
- “Diabetic foot” OR “Pie diabético”.
- “Ultrasound imaging” OR “Imagen por ultrasonido”.
Search strategies
- 1 AND 2.
- 1 AND 3.
- 1 AND 4.
- 1 AND 5.
- 1 AND (3 OR 4 OR 5).
- (1 OR 6) AND 2 AND (3 OR 4 OR 5).
Study selection process
Two independent reviewers screened the titles and abstracts of studies identified through the search. Selected studies were then evaluated in full to determine final eligibility. Any disagreements were resolved through discussion or consultation with a third reviewer.
Data extraction
- The following data were collected:
- General study information (author, year, country, design)
- Population characteristics (age, sex, diagnosed condition)
- Description of the intervention (type of elastography used, pathology assessed)
- Clinical outcomes (sensitivity, specificity, correlation with other diagnostic methods, clinical impact)
- Limitations reported by authors
Specific tools were used to assess risk of bias: the Cochrane Risk of Bias Tool for clinical trials and de Newcastle. Ottawa Scale for Observational studies.
Synthesis of results
A meta-analysis was conducted if study heterogeneity allowed. Otherwise, a structured narrative synthesis was provided. Heterogeneity was measured using the I² statistic. Qualitative and quantitative data were compared and grouped by elastography technique and evaluated pathology.
Results
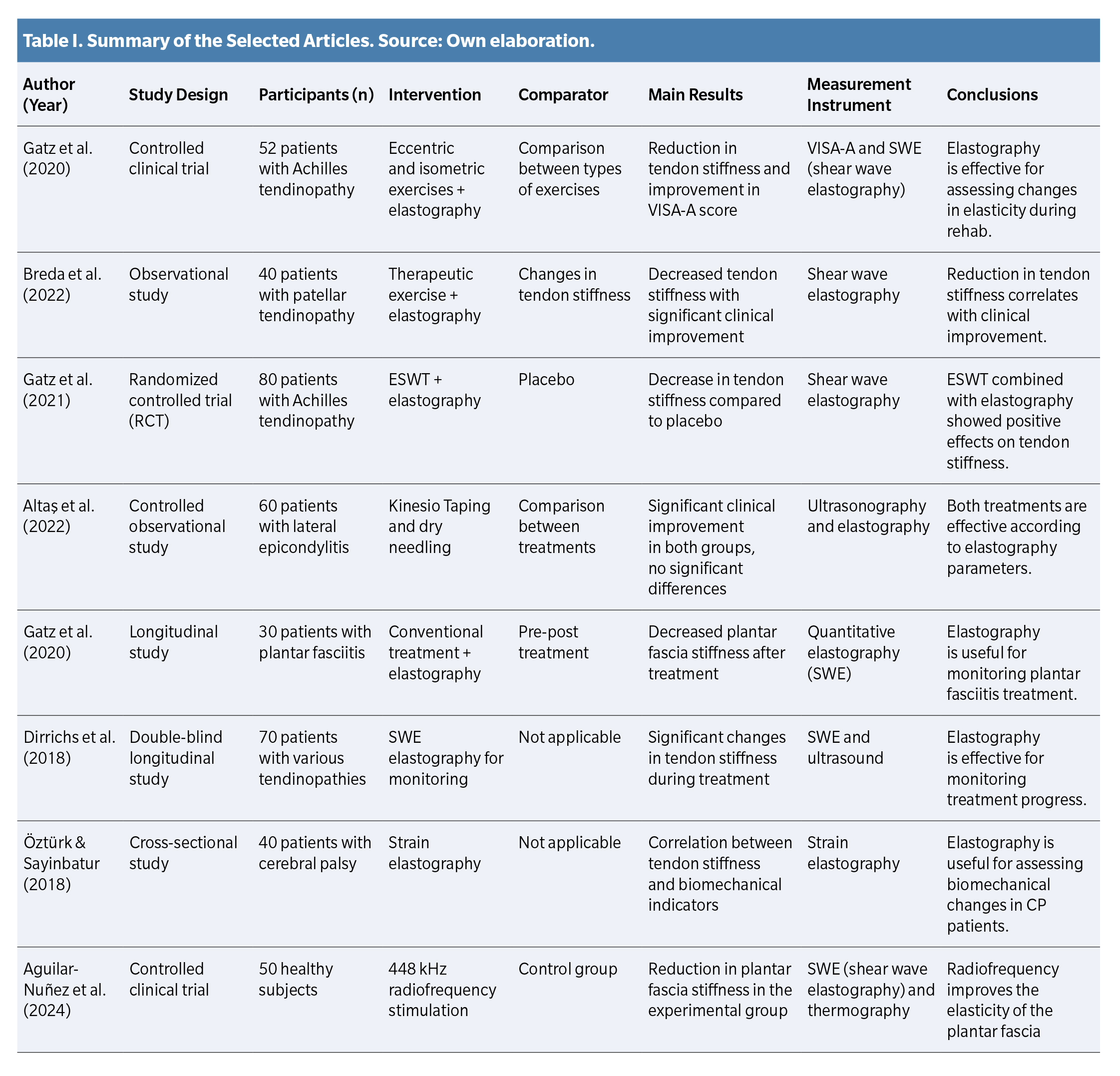
A detailed analysis of the selected studies is presented below, including key information on study design, participant characteristics, interventions, comparison groups, main findings, and outcome measurement instruments. For better visualization, data are summarized in Table 1.
Characteristics of Selected Studies
The included studies feature diverse methodological designs, such as randomized controlled trials, observational studies, and both cross-sectional and longitudinal studies. In total, the sample includes patients with various musculoskeletal pathologies, including Achilles tendinopathy, patellar tendinopathy, lateral epicondylitis, plantar fasciitis, and biomechanical abnormalities in patients with cerebral palsy. Additionally, one study included healthy subjects to assess the effects of radiofrequency stimulation.
Interventions included exercise therapies (eccentric and isometric), dry needling, kinesiotaping, extracorporeal shock wave therapy (ESWT), radiofrequency, and monitoring via elastography. Comparators varied and included placebo groups, no-intervention controls, and comparisons between different therapeutic modalities.
Clinical outcomes and assessment of musculoskeletal elasticity
Main findings show that shear wave elastography (SWE) is an effective tool to evaluate changes in tendon and muscle stiffness in response to different treatments. Gatz et al. (2020, 2021) demonstrated a significant reduction in Achilles tendon stiffness after eccentric and isometric exercises, with even greater improvement when ESWT was combined with elastography.
Breda et al. (2022) reported a positive correlation between decreased patellar tendon stiffness and clinical improvement, while Altas et al. (2022) found significant improvement in patients with lateral epicondylitis treated with kinesiotaping and dry needling, with no significant differences between the two treatments.
Aguilar-Nuñez et al. (2024) demonstrated that 448 kHz radiofrequency stimulation in healthy subjects produced a significant reduction in plantar fascia stiffness, supporting its potential therapeutic use.
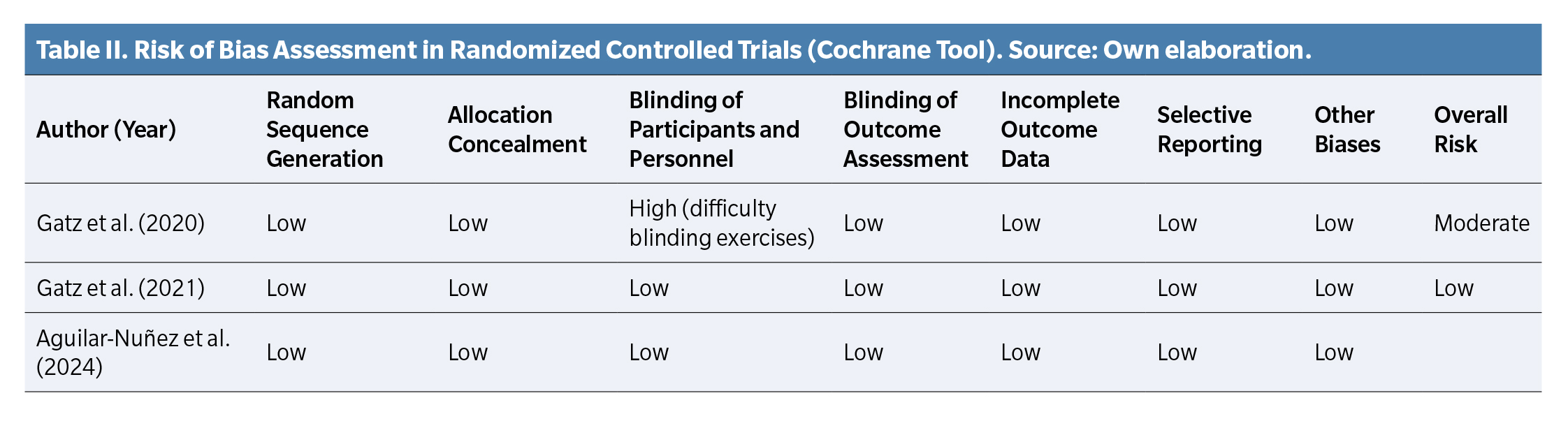
Risk of bias and methodological quality assessment
To assess methodological quality of randomized controlled trials, the Cochrane risk of bias tool was used (Table 2). Moderate risk was identified in Gatz et al. (2020) due to difficulty blinding exercise interventions, while Gatz et al. (2021) and Aguilar-Nuñez et al. (2024) showed low risk across all assessed categories.
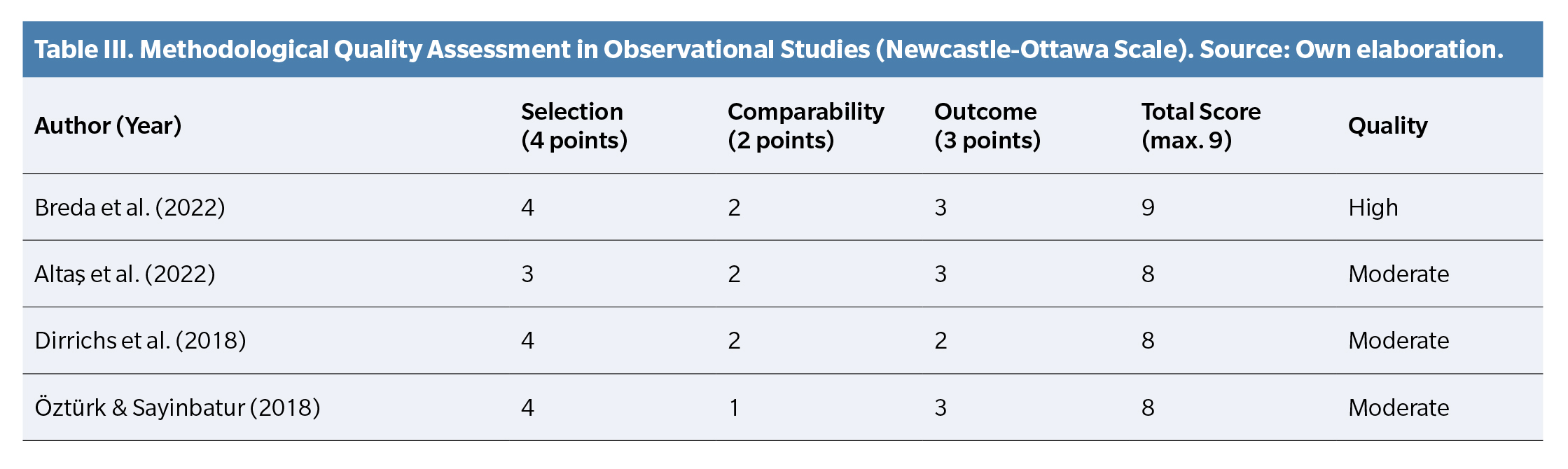
For observational studies, the Newcastle-Ottawa Scale was applied (Table 3). Breda et al. (2022) and Dirrichs et al. (2018) scored highly, while Alta? et al. (2022) and Öztürk & Sayinbatur (2018) showed moderate methodological quality.
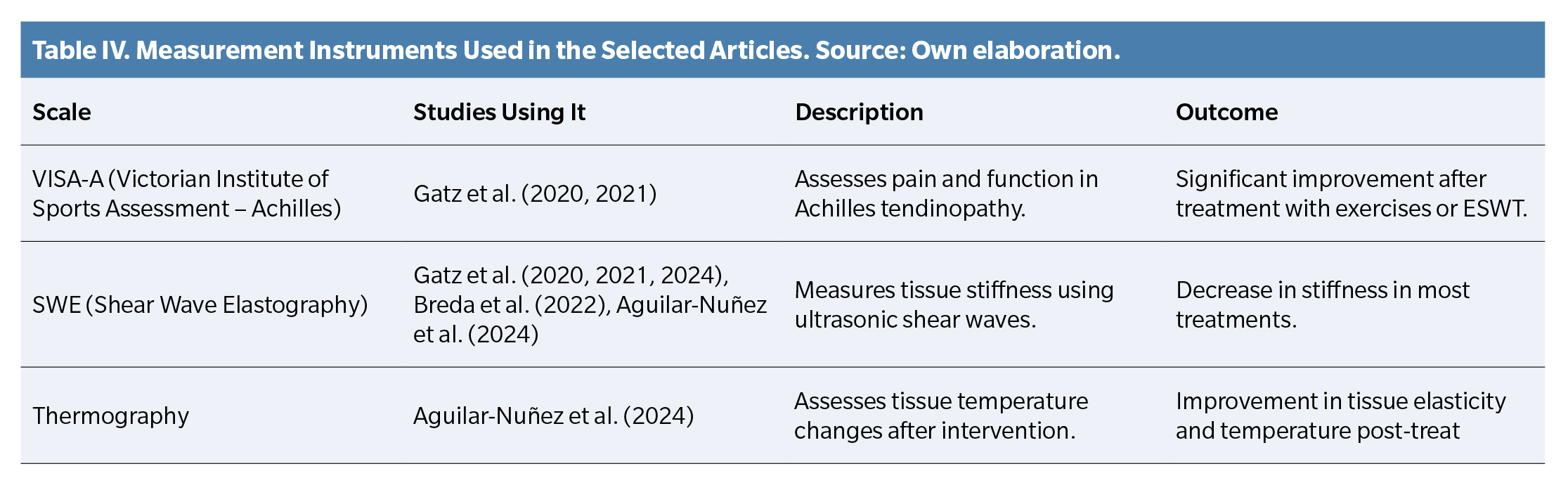
Measurement instruments used
The selected studies used various tools for clinical and functional assessment (Table 4), including:
- VISA-A: Used in Achilles tendinopathy studies to assess pain and function
- SWE (Shear Wave Elastography): Used in most studies to measure musculoskeletal tissue stiffness
- Thermography: Used to assess post-treatment tissue temperature changes
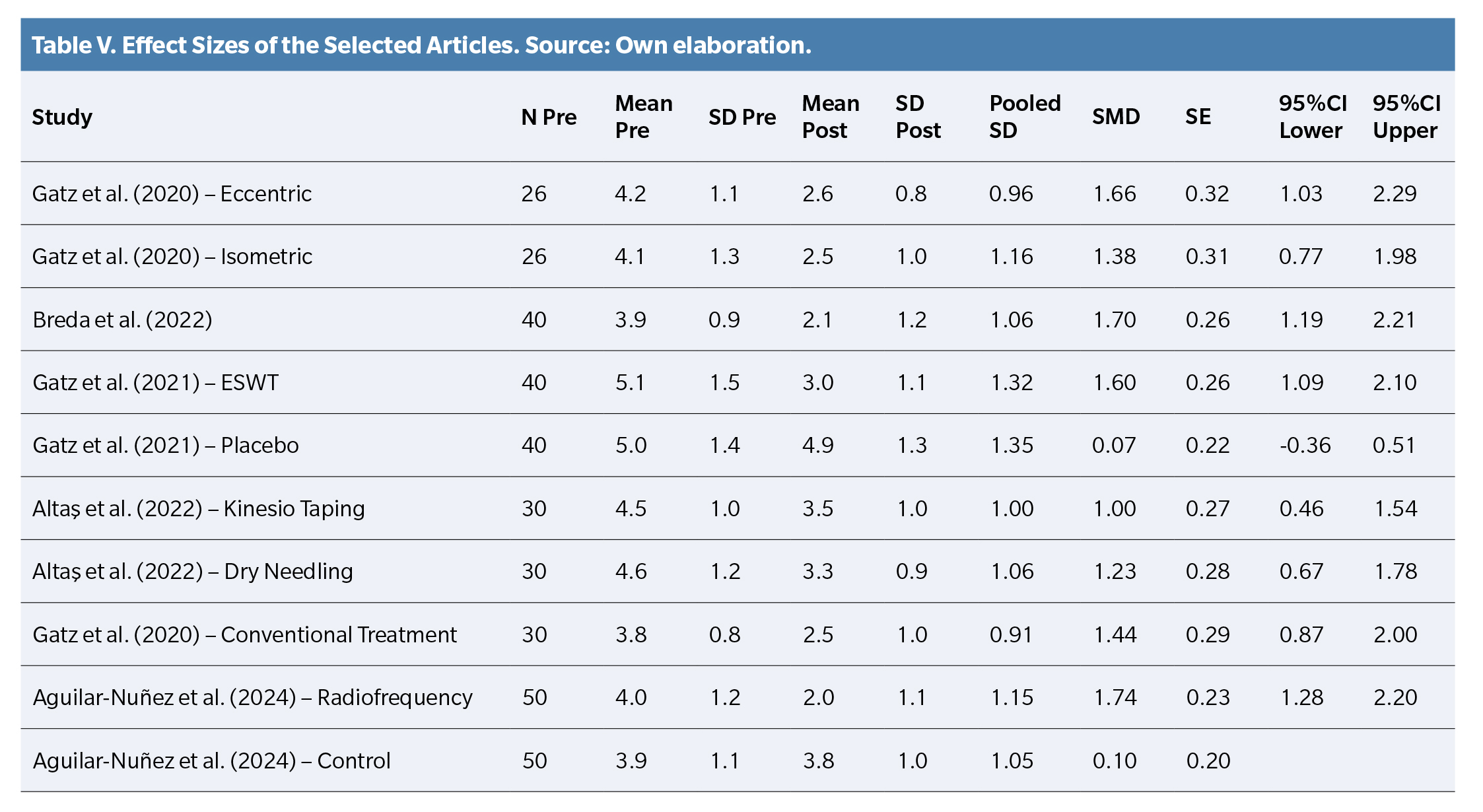
Effect size analysis
Effect sizes were calculated using the Standardized Mean Difference (SMD), with positive and significant values found in most studies, indicating improvements in tendon stiffness and patient functionality (Table 5).
A Forest Plot (Figure 1) was created to visually represent results, showing that elastography-based treatments had a significant positive effect in most cases. Placebo and control groups showed effect sizes near zero, confirming the absence of significant changes in these groups.
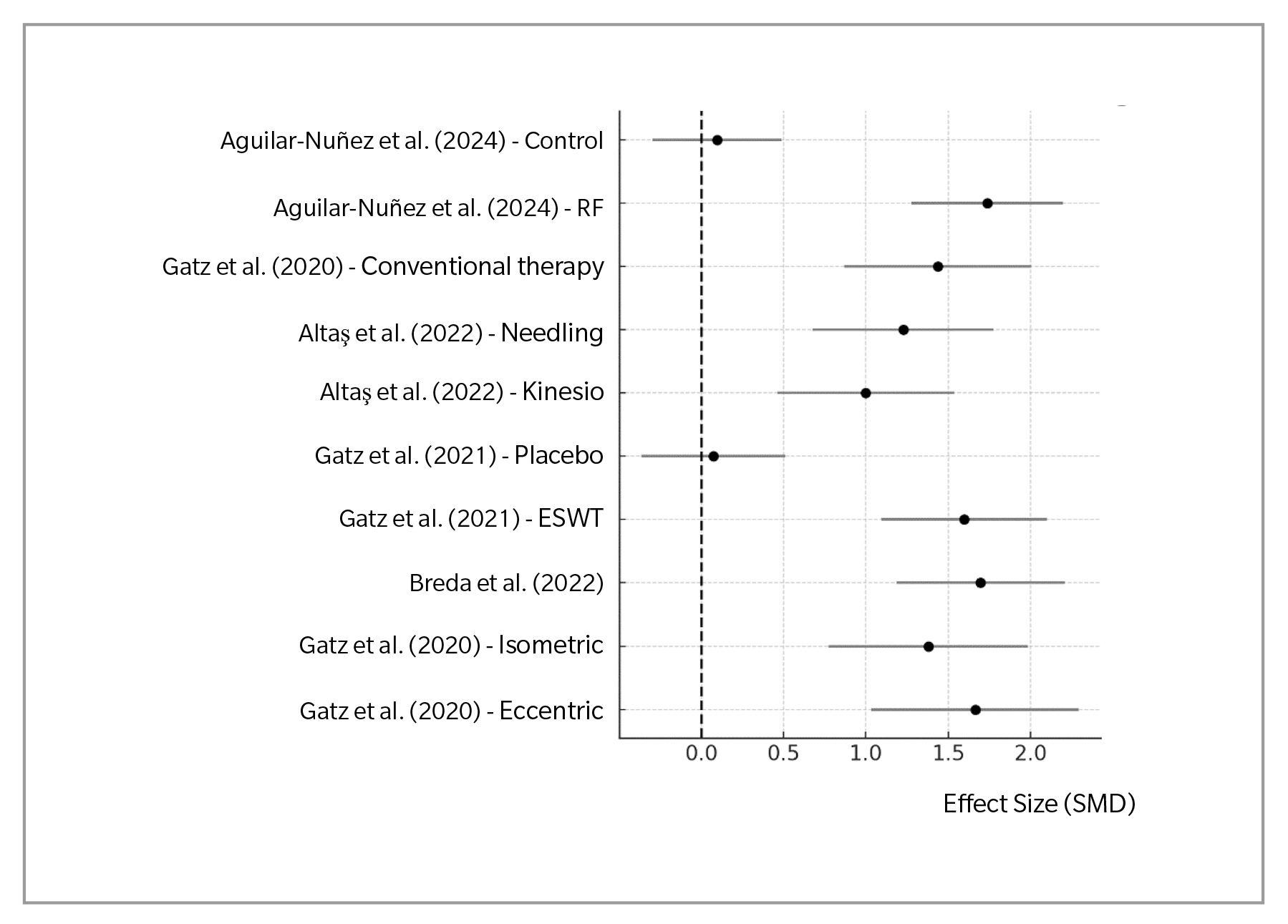
Figure 1. Forest Plot. Effect Size in Interventions (Elastography in Podiatry).
Discussion
Based on the references included in this systematic review the results show how elastography has been used to evaluate and monitor various podiatric and musculoskeletal conditions, particularly tendinopathies and plantar fasciitis.
In 2020, Gatz et al. (13,14) evaluated the effectiveness of eccentric and isometric exercises in patients with Achilles tendinopathy using shear wave elastography (SWE). The results showed a significant reduction in tendon stiffness with both types of exercises, which correlated with improvements in VISA-A scores (a score used to assess pain and function in Achilles tendinopathy). Elastography proved to be a useful tool for monitoring biomechanical changes in the tendon associated with physical therapy.
A year later, in 2021, Gatz et al. (15) conducted a randomized controlled trial that assessed extracorporeal shockwave therapy (ESWT) in patients with Achilles tendinopathy, using elastography to monitor changes in tendon stiffness. The results indicated that ESWT significantly reduced tendon stiffness compared to the placebo group, supporting the use of elastography as a tool for monitoring non-invasive therapies.
In 2018, Öyinbatur and Sayinbatur(20) investigated the relationship between biomechanical indicators and strain ratio of the Achilles tendon in patients with cerebral palsy using strain elastography. They found that the strain index correlated with tendon stiffness and foot functionality, suggesting that elastography could be useful for evaluating biomechanical alterations in populations with neuromuscular disabilities.
In 2022, Breda et al. (16) studied the decrease in patellar tendon stiffness during an exercise therapy program for patellar tendinopathy using elastography. Their findings showed that the reduction in tendon stiffness during treatment was associated with clinical improvement in patients. Elastography was a key tool for objectively measuring changes in the tendon throughout the course of treatment.
Other authors, such as Gatz et al(13,14) in 2020, used elastography to monitor plantar fasciitis treatment. In a group of patients receiving conventional therapy, a decrease in plantar fascia stiffness was observed after treatment, correlating with improvements in pain and function. The authors concluded that elastography is useful for tracking therapeutic responses in plantar fasciitis, enabling non-invasive evaluation of tissue changes.
In 2024, Aguilar-Nuñez et al. (18) reported the short-term effects of 448 kHz radiofrequency stimulation on the plantar fascia using quantitative elastography and thermography. The study showed an immediate decrease in plantar fascia stiffness in healthy subjects, suggesting that this technique may be effective as a physical therapy to improve soft tissue elasticity. This study supports the utility of elastography as a monitoring tool in novel therapies.
Authors such as Dirrichs et al. (19), in 2018, conducted a double-blind longitudinal study that assessed the use of elastography for monitoring the treatment of various tendinopathies, including Achilles tendinopathy and plantar fasciitis. The findings demonstrated that elastography is a useful tool to monitor changes in tendon stiffness during treatment, offering objective data that complements conventional clinical evaluation.
In 2019, Brage et al. (21) evaluated the intra- and inter-observer reliability of strain elastography to detect abnormalities in the supraspinatus tendon. Although this study did not focus directly on podiatry, its findings on elastography reliability could be extrapolated to other body areas, including the feet. Elastography showed good inter-observer reliability, supporting its use as a reproducible diagnostic technique.
Finally, in 2022, authors such as Alta? et al. (17) compared the effectiveness of Kinesio Taping and dry needlingin the treatment of lateral epicondylitis, using ultrasonography and elastography as evaluation tools. Although this study is not directly related to podiatry, it underscores the importance of elastography in comparing different non-invasive therapeutic approaches—a methodology also applicable in podiatric practice.
Limitations
There is possible heterogeneity among the selected studies regarding the type of elastography technique employed. Elastography includes various modalities such as shear wave elastography (SWE) and strain elastography, which differ in precision, sensitivity, and reliability when assessing tissues. This technical diversity may lead to variability in results and hinder direct comparison between studies.
Moreover, differences in the clinical conditions evaluated (e.g., plantar fasciitis, tendinopathies, neuromas) may increase heterogeneity, limiting the ability to draw generalizable conclusions about the effectiveness of elastography in the diagnosis or treatment of podiatric conditions.
The results of the review may have limited clinical applicability if most of the included studies focus on a single condition, such as plantar fasciitis, to the detriment of other common foot and ankle disorders. This focus may bias the conclusions and make it difficult to extrapolate findings to other conditions that could benefit from elastography. Additionally, the lack of adequate representation of a variety of pathologies limits the overall clinical utility of the results and the potential for recommending routine use of elastography in podiatric practice.
Many studies may use different protocols to perform elastography, including variations in applied pressure, tissue depth assessed, and measurement points. These differences may affect the reproducibility of results and complicate the performance of a robust meta-analysis. The lack of consensus on technical and clinical parameters for elastography in podiatry represents a barrier to standardizing its use in evaluating foot pathologies.
Conclusions
The reviewed studies highlight elastography as a useful and reliable tool for monitoring changes in tendon and muscle stiffness during treatment of various musculoskeletal disorders. A positive correlation was observed between the reduction in tissue stiffness and clinical improvement in patients with tendinopathies and plantar fasciitis, as well as potential usefulness in biomechanical evaluation of patients with cerebral palsy. These findings support the use of elastography as a complementary tool in the evaluation and follow-up of physiotherapeutic and podiatric treatments, opening the door to new lines of research in this field.
Authors’ contributions
Study conception and design: AMRP
Data collection: AMRP, RGP
Analysis and interpretation of results: RRM, FJRC
Draft writing and preparation: RRM, FJRC
Final review: RGP
Funding
None declared.
Conflicts of interest
None declared.
References
- Bell EA, Hibbert JE, Domire ZJ. Measurement of intrinsic foot stiffness in minimally and traditionally shod runners using ultrasound elastography: A pilot study. J Sports Sci. 2020;38(13):1516-23. DOI: 10.1080/02640414.2020.1746595.
- Hirota K, Watanabe K, Miyamoto H, Negishi K, Watase M, Teramoto A. Comparison by ultrasound shear wave elastography of toe flexor muscle contraction during MTP flexion exercise and short-foot exercise. J Back Musculoskelet Rehabil. 2024;37(4):1041-7. DOI: 10.3233/BMR-230282.
- Lung CW, Wu FL, Liao F, Pu F, Fan Y, Jan YK. Emerging technologies for the prevention and management of diabetic foot ulcers. J Tissue Viability. 2020;29(2):61-8. DOI: 10.1016/j.jtv.2020.03.003.
- Gonzalez FM, Gleason CA, Lee KS, Labid SA, Nazarian LN, Morrison WB, et al. Shear Wave Elastography assessment and comparison study of the Achilles tendons in optimally conditioned asymptomatic young collegiate athletes. Skeletal Radiol. 2021;50(12):2381-92. DOI: 10.1007/s00256-021-03798-5.
- Rougereau G, Marty-Diloy T, Vigan M, Donadieu K, Hardy A, Vialle R, et al. Anatomical and biomechanical study of the inferior extensor retinaculum by Shear-Wave Elastography in healthy adults. Surg Radiol Anat. 2022;44(2):245-52. DOI: 10.1007/s00276-022-02884-0.
- Wu CH, Chiu YH, Chang KV, Wu WT, Özçakar L. Ultrasound elastography for the evaluation of plantar fasciitis: A systematic review and meta-analysis. Eur J Radiol. 2022;155:110495. DOI: 10.1016/j.ejrad.2022.110495.
- Patwari M, Chatzistergos P, Sundar L, Chockalingam N, Ramachandran A, Naemi R. A quantitative comparison of plantar soft tissue strainability distribution and homogeneity between ulcerated and non-ulcerated patients using ultrasound strain elastography. Proc Inst Mech Eng H. 2022;236(5):722-9. DOI: 10.1177/09544119221074786.
- Marouvo J, Sousa F, André MA, Castro MA. Tibialis posterior muscle stiffness assessment in flat foot subjects by ultrasound based Shear-Wave Elastography. Foot (Edinb). 2023;54:101975. DOI: 10.1016/j.foot.2023.101975.
- Schillizzi G, Alviti F, D’Ercole C, Elia D, Agostini F, Mangone M, et al. Evaluation of plantar fasciopathy Shear Wave Elastography: A comparison between patients and healthy subjects. J Ultrasound. 2021;24(4):417-22. DOI: 10.1007/s40477-020-00474-7.
- Mifsud T, Gatt A, Micallef-Stafrace K, Chockalingam N, Padhiar N. Elastography in the assessment of the Achilles tendon: A systematic review of measurement properties. J Foot Ankle Res. 2023;16(1):23. DOI: 10.1186/s13047-023-00623-1.
- Zhang F, Wang J, Ma Y, Wang Y, Wang W, Wang Y. Evaluation of Achilles tendon in patients with diabetic foot ulcer by high-frequency ultrasound combined with real-time Shear-Wave Elastography. J Healthc Eng. 2022;2022:4866240. DOI: 10.1155/2022/4866240.
- Kandil NM, Hashem AMB, Toukhy MME, Yousef NMAA, Al-Feeshawy ASH, Havwana MAR. Ultrasound imaging and Shear Wave Elastography for the differential diagnosis of heel pain: A comparative cross-sectional study. J Ultrasound. 2024;27(3):621-34. DOI: 10.1007/s40477-024-00906-8.
- Gatz M, Betsch M, Dirrichs T, Schrading S, Tingart M, Michalik R, et al. Eccentric and isometric exercises in Achilles tendinopathy evaluated by the VISA-A Score and shear wave elastography. Sports Health. 2020;12(4):373-81. DOI: 10.1177/1941738119893996.
- Gatz M, Betsch M, Quack V, Bejder L, Schrading S, Tingart M, et al. Shear wave elastography for treatment monitoring of plantar fasciitis. J Sports Med Phys Fitness. 2020;60(8):1137-47. DOI: 10.23736/S0022-4707.20.10702-3.
- Gatz M, Schweda S, Betsch M, Dirrichs T, de la Fuente M, Reinhardt N, et al. Line- and point-focused extracorporeal shock wave therapy for Achilles tendinopathy: A placebo-controlled RCT study. Sports Health. 2021;13(5):511-8. DOI: 10.1177/1941738121991791.
- Breda SJ, de Vos RJ, Krestin GP, Oei EHG. Decreasing patellar tendon stiffness during exercise therapy for patellar tendinopathy is associated with better outcome. J Sci Med Sport. 2022;25(5):372-78. DOI: 10.1016/j.jsams.2022.01.002.
- Altas EU, Birlik B, Sahin Onat S, Özogul Öz B. The comparison of the effectiveness of Kinesio Taping and dry needling in the treatment of lateral epicondylitis: A clinical and ultrasonographic study. J Shoulder Elbow Surg. 2022;31(8):1553-62. DOI: 10.1016/j.jse.2022.03.010.
- Aguilar-Nuñez D, Cervera-Garvi P, Gonzalez-Muñoz A, Navarro-Ledesma S. Short-term effects of 448 kilohertz radiofrequency stimulation on plantar fascia measured by quantitative ultrasound elastography and thermography on active healthy subjects: an open controlled clinical trial. Int J Hyperthermia. 2024;41(1):2366429. DOI: 10.1080/02656736.2024.2366429.
- Dirrichs T, Quack V, Gatz M, Tingart M, Rath B, Betsch M, et al. Shear Wave Elastography (SWE) for monitoring of treatment of tendinopathies: A double-blinded, longitudinal clinical study. Acad Radiol. 2018;25(3):265-72. DOI: 10.1016/j.acra.2017.09.011.
- Öztürk M, Sayinbatur B. Real-time ultrasound elastography of the Achilles tendon in patients with cerebral palsy: is there a correlation between strain ratio and biomechanical indicators? J Med Ultrason (2001). 2018;45(1):143-48. DOI: 10.1007/s10396-017-0800-y.
- Brage K, Hjarbaek J, Kjaer P, Ingwersen KG, Juul-Kristensen B. Ultrasonic strain elastography for detecting abnormalities in the supraspinatus tendon: An intra- and inter-rater reliability study. BMJ Open. 2019;9(5):e027725.