doi.org/10.20986/revesppod.2026.1765/2025
ORIGINAL
Pain assessment and effectiveness of anesthetic procedures in patients with onychocryptosis undergoing nail surgery: a randomized clinical trial
Evaluación del dolor y efectividad de los procedimientos anestésicos en pacientes con onicocriptosis sometidos a cirugía ungueal: ensayo clínico aleatorizado
Ana M.ª Rayo Pérez1
Rafael Rayo Martín1
Rafael Rayo Rosado1
Joao Miguel Costa Martiniano2
Raquel García de la Peña1
1Departamento de Podología. Universidad de Sevilla, España
2Escola Superior de Saúde da Cruz Vermelha Portuguesa. Lisboa, Portugal
Abstract
Introduction: Local anesthesia is essential in podiatric surgery; however, anesthetic infiltration often causes pain and anxiety in patients. The choice of injection technique and administration method may influence pain perception, especially in digital hallux block.
Patients and methods: A randomized, single-blind clinical trial was conducted with 120 patients undergoing nail surgery for onychocryptosis. Participants were randomly assigned to 4 groups based on the anesthetic technique (Frost’s H or modified Frost’s H) and the administration method (conventional syringe or carpule). 3 % mepivacaine was used, and postinfiltration pain was measured using the Visual Analog Scale (VAS). Statistical analysis included nonparametric tests (Kruskal-Wallis and Mann-Whitney U).
Results: The modified H of Frost technique showed lower pain scores compared to the conventional technique (mean VAS: 3.8 vs. 4.3; p = 0.045). The use of carpule significantly reduced pain perception compared to the conventional syringe (mean VAS: 3.7 vs. 4.4; p = 0.023).
Conclusion: The modified H of Frost technique and the use of carpule improve patient tolerance to anesthetic infiltration, representing useful strategies to optimize the clinical experience in podiatric surgery.
Keywords: First ray, foot, plantar flexion, dorsal flexion, total mobility, low back pain
Resumen
Introducción: La anestesia local es fundamental en cirugía podológica, pero la infiltración anestésica suele generar dolor y ansiedad en los pacientes. La elección de la técnica de inyección y del método de administración puede influir en la percepción dolorosa, especialmente en el bloqueo digital del hallux.
Pacientes y métodos: Se llevó a cabo un ensayo clínico aleatorizado y simple ciego con 120 pacientes sometidos a cirugía ungueal por onicocriptosis. Los participantes fueron asignados al azar a 4 grupos según la técnica anestésica (H de Frost o H de Frost modificada) y el método de administración (jeringa convencional o carpule). Se utilizó mepivacaína al 3 % y el dolor postinfiltración se midió mediante la Escala Visual Analógica (EVA). El análisis estadístico incluyó pruebas no paramétricas (Kruskal-Wallis y U de Mann-Whitney).
Resultados: La técnica de H de Frost modificada presentó menor dolor en comparación con la técnica convencional (media EVA: 3.8 vs. 4.3; p = 0.045). El uso de carpule redujo significativamente la percepción dolorosa frente a la jeringa convencional (media EVA: 3.7 vs. 4.4; p = 0.023).
Conclusión: La técnica de H de Frost modificada y el uso de carpule mejoran la tolerancia del paciente a la infiltración anestésica, constituyendo estrategias recomendables para optimizar la experiencia clínica en cirugía podológica.
Palabras claves: Anestesia local, dolor, infiltración anestésica, analgesia tópica, cirugía podológica, dedo, pie, onicocriptosis
Corresponding autor
Ana M.ª Rayo Pérez
anarayo43@gmail.com
Received: 29-09-2025
Accepted: 02-12-2025
Introduction
the administration of local anesthesia is a fundamental procedure in multiple medical and surgical specialties, including podiatry, dermatology, and dentistry. However, anesthetic infiltration often causes pain and anxiety in patients, which has driven the development of strategies aimed at reducing discomfort and improving the overall clinical experience(1,2). The perception of pain during injection depends on several factors, such as the infiltration technique used, needle gauge, volume and speed of administration, as well as the use of topical agents or adjuvant physical methods(3,4).
Various approaches intended to mitigate pain associated with anesthetic infiltration have been described in the literature. Among them, local cooling or cold air has demonstrated efficacy in nail surgery by improving tolerance to the procedure(5). Similarly, specific needle-insertion techniques—such as parallel puncture to the skin plane or minimal insertion—have been proposed to reduce pain perception¹. The choice of anesthetic agent is also relevant: the addition of epinephrine can prolong block duration and improve its effectiveness, although with interindividual variability(7).
Pain sensitivity is not homogeneous and may vary depending on factors such as age or the patient’s emotional state. It has been documented that pain perception tends to decrease with age, which may explain significant differences between age groups(7). Furthermore, pre-procedural anxiety can exacerbate pain perception, highlighting the importance of implementing strategies that reduce both physical discomfort and psychological burden(8).
In hallux surgery, specific digital nerve block techniques have been developed to optimize effectiveness and reduce discomfort during infiltration. The “V” technique has shown satisfactory results in procedures such as onychocryptosis(9). In parallel, the application of topical anesthetics—such as 20% benzocaine—has demonstrated variable effectiveness in reducing pre-infiltration pain, with inconsistent results across studies(10,11).
The persistence of pain associated with infiltrative anesthesia remains a relevant clinical challenge. For this reason, it is essential to continue investigating strategies that combine less invasive techniques, complementary physical and pharmacological methods, and individualized anesthetic approaches based on patient characteristics. Advances in these areas would not only improve the anesthetic experience but also enhance the safety, effectiveness, and overall satisfaction with the surgical procedure. The present study aims to evaluate the pain perceived during anesthetic infiltration in patients with onychocryptosis undergoing nail surgery using the phenol-alcohol technique, comparing different block techniques (H of Frost and modified H of Frost) and administration methods (conventional syringe or carpule). Additionally, we examined the possible influence of sex and the result of the Prick Test on pain intensity, measured through the Visual Analogue Scale (VAS).
Patients and methods
Design
We conducted a randomized, single-blind, factorial 2×2 clinical trial, following the Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Participants
Participants were randomly assigned using a computer-generated sequence into one of four experimental groups, ensuring homogeneity in terms of sex and age through block randomization (block size: 4). Allocation concealment was achieved using opaque, numbered, sealed envelopes prepared by an independent investigator.
The experimental groups were as follows: 1) H of Frost technique with conventional syringe; 2) H of Frost technique with carpule; 3) Modified H of Frost technique with conventional syringe; and 4) Modified H of Frost technique with carpule.
Each group consisted of 30 participants (n = 120). The study followed a single-blind scheme, such that patients were unaware of the infiltration technique assigned.
Recruitment took place at Clínica Rayo (Arahal, Seville, Spain) between January and December 2023/2024. Potential participants were informed about the study during their pre-surgical consultation and invited to participate voluntarily.
Eligibility criteria
Inclusion criteria were adults aged 18–40 years with unilateral onychocryptosis requiring digital surgery using the phenol-alcohol technique, who provided signed informed consent.
Exclusion criteria included allergy to local anesthetics, active infection at the surgical site, peripheral neurological or vascular disorders, pregnancy, or breastfeeding.
Study variables
The primary variable was pain intensity immediately after anesthetic infiltration, assessed using the 10-cm VAS (0 = “no pain,” 10 = “unbearable pain”).
The secondary variable was the response to the Prick Test at 5 minutes post-infiltration, consisting of a superficial puncture with a sterile needle to evaluate the presence or absence of pain sensitivity in the anesthetized area, serving as an objective measure of block effectiveness.
Demographic variables were also recorded: age, sex, and laterality of the operated foot.
The VAS was administered on paper, self-completed by the patient immediately after infiltration, following instructions to mark the perceived pain intensity during the injection.
Techniques and procedures
All procedures were performed by a single operator with more than 5 years of experience in podiatric surgery, under controlled environmental conditions: an average temperature of 20.4 °C, relative humidity of 55 %, uniform lighting, and ergonomic positioning of the patient with the foot resting on a padded support. Two infiltration methods (conventional syringe and carpule) were used, applied through two anesthetic techniques:
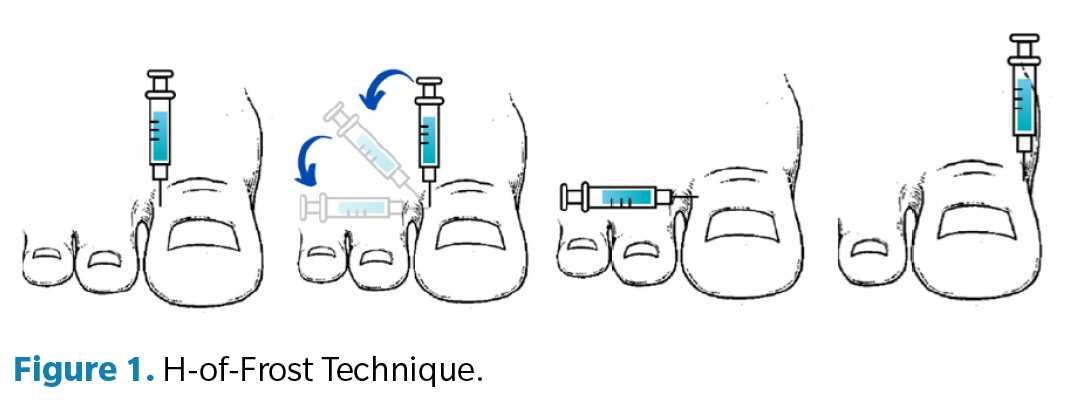
- H-Frost technique (Figure 1): 2 punctures are performed at 90° to the axis of the toe to block the digital nerves of the hallux. First, a puncture is performed at the lateral base of the toe, depositing an anesthetic wheal in the plantar region and creating an anesthetic track toward the dorsal area. Next, with the toe in slight dorsiflexion, the needle is inserted above the tendon of the extensor hallucis longus to infiltrate a second anesthetic wheal at its medial base. Finally, a second puncture is made at the medial base of the toe, depositing a plantar anesthetic wheal and completing the anesthetic track toward the dorsal region¹.
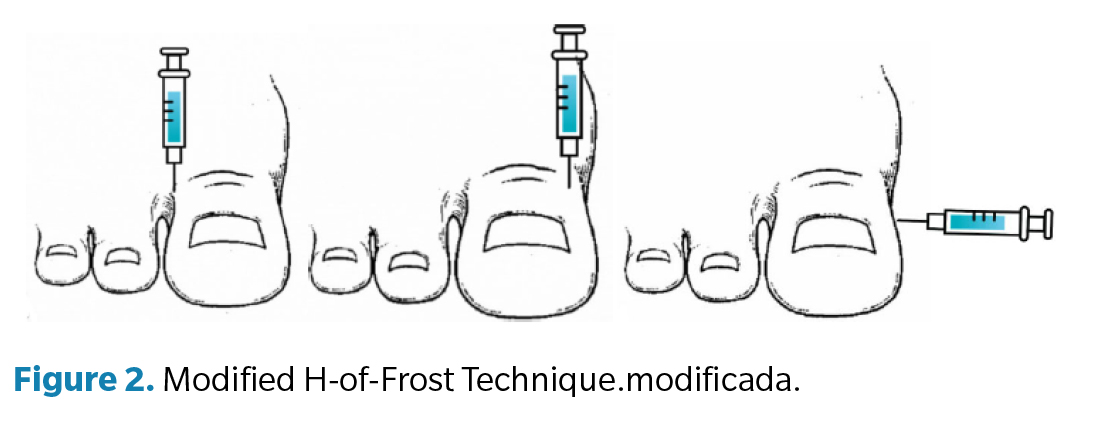
- Modified H-Frost technique (Figure 2): 3 punctures are performed at 90° to the axis of the toe. First, a puncture is performed at the lateral base of the toe, depositing an anesthetic wheal in the plantar region and creating an anesthetic track toward the dorsal area. Then, a 2nd puncture is performed at the medial base of the toe, depositing a plantar anesthetic wheal and completing the dorsal anesthetic track. Finally, a third puncture is carried out at the medial–plantar base of the toe, depositing an anesthetic track from plantar–lateral to plantar–medial¹².
A constant volume of 3.8 mL of 3 % mepivacaine without vasoconstrictor was administered in all infiltrations, using a 27 G needle measuring 40 × 25 mm to ensure procedural uniformity. This volume was obtained using two carpule-type vials per infiltration, since each carpule contained 1.6 mL of anesthetic solution.
Pain intensity was recorded immediately after the infiltration using the VAS (Visual Analog Scale), without the evaluator knowing which technique had been applied, ensuring partial blinding during data collection.
Sample size
The sample size was set at 120 patients (30 per group), calculated to detect a minimum difference of 1.5 points on the VAS, with a statistical power of 80 % and a significance level of 0.05, assuming a standard deviation of 2 points.
Statistical analysis
Continuous variables were described using mean ± standard deviation or median (interquartile range) depending on their distribution. Normality was checked with the Shapiro–Wilk test. For group comparisons, hypothesis tests using non-parametric methods (Kruskal–Wallis and Mann–Whitney U tests with Bonferroni correction) were applied; 95% confidence intervals and effect sizes (Rosenthal’s r) were calculated to assess the clinical relevance of observed differences. Additionally, a multivariate logistic regression analysis was performed to identify factors associated with post-infiltration pain. All analyses were conducted using SPSS v.25 (IBM Corp., Armonk, NY, USA), with statistical significance set at p < 0.05.
Results
A descriptive analysis of the variables included in the study (Table 1) was performed to characterize the sample and establish the basis for inferential analyses.
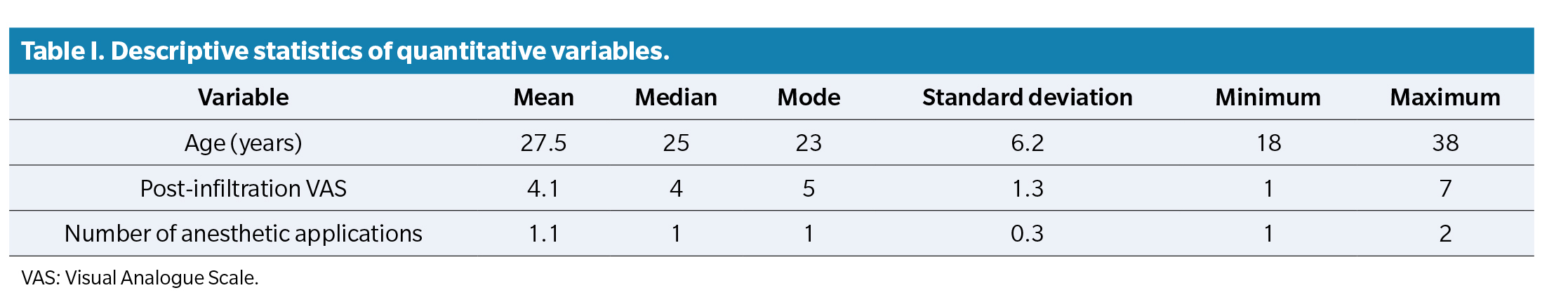
Pain intensity after infiltration, measured using the VAS, showed a mean of 4.1, median of 4, and mode of 5, with a range from 1 to 7 and a standard deviation of 1.3.
In cases of insufficient blocks, the number of required anesthetic applications showed a mean of 1.1, median and mode of 1, with a range from 1 to 2 and a standard deviation of 0.3.
Results indicated that both variables were not normally distributed. For this reason, non-parametric tests were used in inferential analyses.
The Kruskal–Wallis test applied to VAS scores according to surgical technique (Table II) showed that the mean VAS score in patients treated with the H-Frost technique was 4.3, while those treated with the modified H-Frost technique had a mean of 3.8, with p = 0.045, indicating statistically significant differences in perceived pain.
Comparison of pain by sex (Table 2), using the Mann–Whitney U test, showed a mean VAS of 4.2 in men and 3.9 in women, without statistical significance (p = 0.32).
Comparison of VAS scores by infiltration method (Table 2) showed that the mean VAS in the syringe group was 4.4, while in the carpule group it was 3.7, with p = 0.023, indicating statistically significant differences.
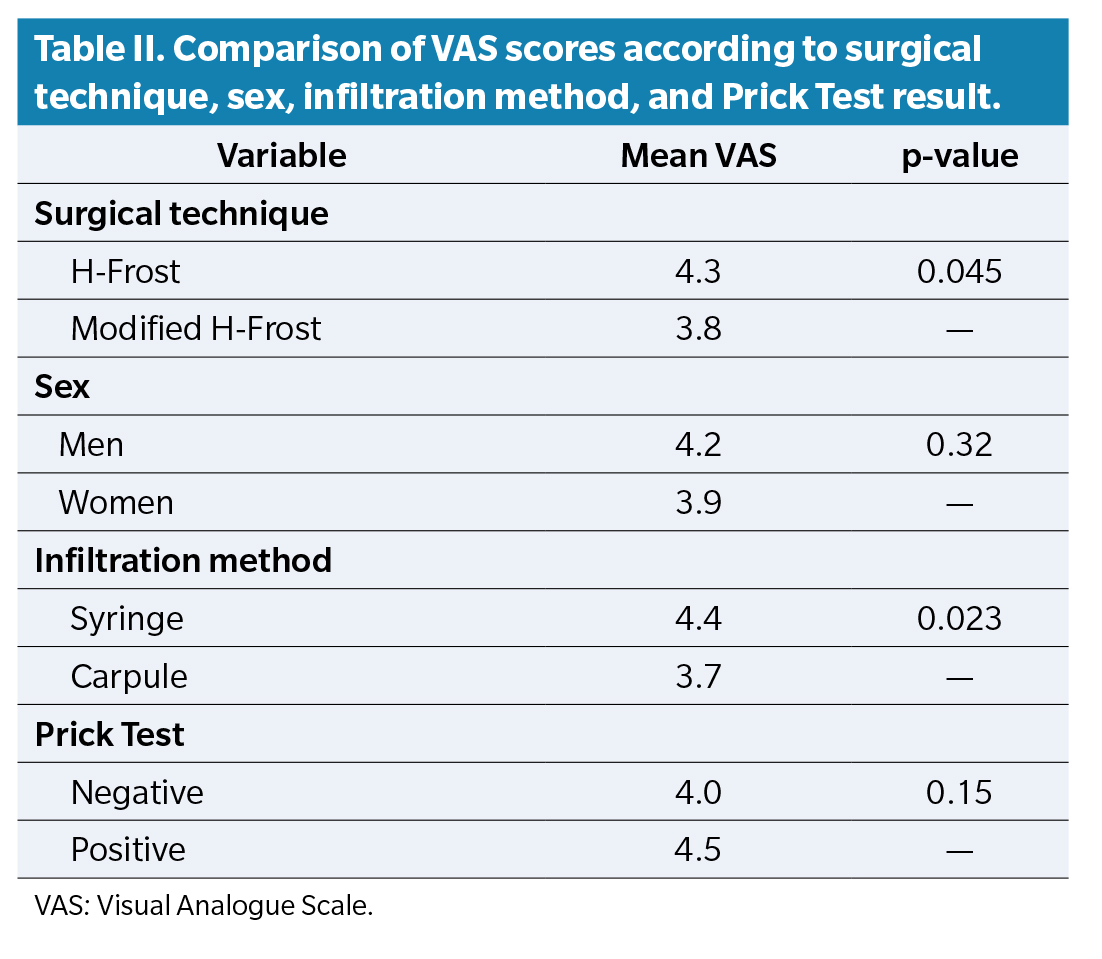
Regarding the Prick Test (Table 2), the mean VAS score was 4.0 in patients with a negative test and 4.5 in patients with a positive test, with no statistical significance (p = 0.15).
Discussion
The pain experienced immediately after anesthetic infiltration is a key factor in determining patient tolerance to minor surgical procedures in podiatry. In the present study, various strategies aimed at reducing the discomfort associated with the administration of local anesthesia were analyzed, yielding results that partially coincide with previous literature and provide new evidence within the specific context of digital podiatric surgery.
The use of topical anesthetics has been the subject of numerous studies. De Freitas et al. (10) demonstrated that 20% benzocaine was more effective than placebo in reducing pain during oral procedures, whereas Al-Melh and Andersson(13) compared different topical agents and concluded that their effectiveness may be limited, particularly in areas of high mucosal sensitivity. Similarly, Serour et al. (14) observed that the application of EMLA cream prior to a digital block did not significantly reduce pain during anesthetic injection. These findings suggest that although topical anesthetics may be useful in certain scenarios, their clinical impact is variable and depends on the type of procedure and the anatomical region treated.
In contrast, cooling agents have shown more consistent and easily applicable efficacy. Kosaraju and Vandewalle(15) found that a refrigerant spray reduced pain more effectively than a topical gel, while Ricardo and Lipner(5) demonstrated that air-cooling significantly improved tolerance during anesthetic infiltration in nail surgery. Consistently, Kose et al. (16) reported a significant reduction in pain following the application of vapocoolants before digital nerve block.
The administration technique is another key factor in pain perception. Martires et al. (17) showed that injecting lidocaine at a 90° angle, instead of 45°, significantly reduced discomfort experienced by patients. Oliveira et al. (18) analyzed the use of needle-free jet injections and concluded that this modality generated less perceived pain than conventional techniques. Likewise, the application of local cold via ice has demonstrated clinical benefits, as documented by Hayward et al. (19), who observed a significant reduction in pain during hallux digital blocks.
The results of the present study are consistent with available evidence, showing that modifying the infiltration technique and applying adjunctive measures can significantly reduce pain perception during infiltrative anesthesia in podiatric surgery. Nevertheless, although topical anesthetics have been widely studied, their effectiveness remains variable, highlighting the need to explore complementary strategies tailored to each clinical situation.
Therefore, future research should focus on identifying the optimal combination of these measures and incorporating the evaluation of other potentially influential factors in patient experience, such as pre-procedure anxiety, individual pain tolerance, and demographic or psychological variables. A multidimensional approach would allow the development of more effective, personalized protocols, helping to improve the anesthetic experience and patient well-being in podiatry.
This study presents several limitations that must be considered when interpreting the results. First, it is a clinical trial conducted at a single center, which may limit the generalizability of the findings to other clinical settings or populations with different sociodemographic or cultural characteristics. Second, although an adequate sample size was obtained to detect significant differences in pain perception, the participant age range (18–40 years) restricts applicability to other age groups, such as pediatric or older adult patients, who may exhibit different pain sensitivity and anesthetic response. Another relevant limitation is the single-blind design: patients were unaware of the assigned infiltration technique, but the investigator was not blinded, which could introduce bias in the administration of anesthesia or data collection. Additionally, psychological variables such as preoperative anxiety—known to influence pain perception—were not assessed, which may have affected the EVA scores obtained. Finally, follow-up was limited to immediate post-infiltration evaluation, without consideration of block duration or potential subsequent complications, restricting analysis of the overall effectiveness of the anesthetic techniques.
In conclusion, the results of this study show that both the infiltration technique and the method of administration significantly influence pain perception during digital anesthesia in patients with onychocryptosis. The modified H-of-Frost technique was associated with lower pain intensity compared to the original technique, and the use of a carpule improved tolerance compared with a conventional syringe. In contrast, no significant differences were observed based on sex or Prick Test outcome, indicating that improvements in patient experience depend primarily on the technical characteristics of the procedure. These findings support the need to optimize anesthetic strategies and suggest that combining the modified technique with carpule use may offer a clinically relevant benefit during anesthetic infiltration.
Ethical statement
The study was registered on ClinicalTrials.gov (NCT06352255) and approved by the Bioethics Research Committee of the Universidad de Málaga (Spain) (code 207-2023-H)
Conflict of interest
None
Funding
None
Authors’ contributions
Study conception and design: RRM. Data collection: AMRP, RRM, RRR. Analysis and interpretation of results: JMCM. Draft creation, writing, and preparation of the initial manuscript: AMRP. Final review: RGP
References
- Zelickson BR, Goldberg LH, Rubenzik MK, Wu WJ, Sinai M. Parallel, minimal needle-insertion technique for achieving a painless injection of local anesthetic. J Am Acad Dermatol. 2017;77(2):369-70. DOI: 10.1016/j.jaad.2017.03.007.
- Strazar AR, Leynes PG, Lalonde DH. Minimizing the pain of local anesthesia injection. Plast Reconstr Surg. 2013;132(3):675-84. DOI: 10.1097/PRS.0b013e31829ad1e2.
- Saenz McPherson J, Dixon SA, Townsend R, Vandewalle KS. Effect of needle design on pain from dental local anesthetic injections. Anesth Prog. 2015;62(1):2-7. DOI: 10.2344/0003-3006-62.1.2.
- Flanagan T, Wahl MJ, Schmitt MM, Wahl JA. Size doesn’t matter: Needle gauge and injection pain. Gen Dent. 2007;55(3):216-7.
- Ricardo JW, Lipner SR. Air cooling for improved analgesia during local anesthetic infiltration for nail surgery. J Am Acad Dermatol. 2021;84(5):e231-2. DOI: 10.1016/j.jaad.2019.11.032.
- Dos Reis Júnior A, Quinto D. Digital block with or without the addition of epinephrine in the anesthetic solution. Braz J Anesthesiol. 2016;66(1):63-71. DOI: 10.1016/j.bjane.2013.12.004.
- Tumi H, Johnson M, Dantas P, Maynard MJ, Tashani OA. Age-related changes in pain sensitivity in healthy humans: A systematic review with meta-analysis. Eur J Pain. 2017;21(6):955-64. DOI: 10.1002/ejp.1011.
- Libonati A, Nardi R, Gallusi G, Angotti V, Caruso S, Coniglione F, et al. Pain and anxiety associated with Computer-Controlled Local Anaesthesia: Systematic review and meta-analysis of cross-over studies. Eur J Paediatr Dent. 2018;19(4):324-32.
- Sánchez Hernández S, Giralt de Veciana E. Anestesia del primer dedo del pie mediante técnica en V en el tratamiento quirúrgico de la onicocriptosis. Actas Dermosifiliogr. 2022;113(4):425-6. DOI: 10.1016/j.ad.2020.08.024.
- De Freiras GC, Pozzobon RT, Blaya DS, Moreira CH. Efficacy of benzocaine 20% topical anesthetic compared to placebo prior to administration of local anesthesia in the oral cavity: A randomized controlled trial. Anesth Prog. 2015;62(2):46-50. DOI: 10.2344/0003-3006-62.2.46.
- Noël B. Letter: Anesthesia for ingrowing toenail surgery. Dermatol Surg. 2010;36(8):1356-7. DOI: 10.1111/j.1524-4725.2010.01640.x.
- Rayo-Pérez AM, Rayo-Rosado R, Rayo-Martín R, Reina-Bueno M. Analysis of pain and effectiveness in digital block of the first toe using syringe vs. carpule: Frost’s H vs. modified Frost’s H randomized clinical trial. J Clin Med. 2024;13(14):4185. DOI: 10.3390/jcm13144185.
- Al-Melh MA, Andersson L. Comparison of topical anesthetics (EMLA/Oraqix vs. benzocaine) on pain experienced during palatal needle injection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(5):e16. DOI: 10.1016/j.tripleo.2006.11.033.
- Serour F, Ben-Yehuda Y, Boaz M. EMLA cream prior to digital nerve block for ingrown nail surgery does not reduce pain at injection of anesthetic solution. Acta Anaesthesiol Scand. 2002;46(2):203-6. DOI: 10.1034/j.1399-6576.2002.460215.x.
- Kosaraju A, Vandewalle KS. A comparison of a refrigerant and a topical anesthetic gel as preinjection anesthetics. J Am Dent Assoc. 2009;140(1):68-72. DOI: 10.14219/jada.archive.2009.0020.
- Kose O, Saylan S, Ediz N, Yigit S. Effects of topical alkane vapocoolant spray on pain intensity prior to digital nerve block for ingrown nail surgery. Foot Ankle Spec. 2010;3(2):73-5. DOI: 10.1177/1938640010363172.
- Martires KJ, Malbasa CL, Bordeaux JS. A randomized controlled crossover trial: Lidocaine injected at a 90-degree angle causes less pain than lidocaine injected at a 45-degree angle. J Am Acad Dermatol. 2011;65(6):1231-3. DOI: 10.1016/j.jaad.2011.04.011.
- Oliveira ACA, Amorim KS, Nascimento Júnior EM, Duarte ACB, Groppo FC, Takeshita WM, et al. Evaluación de las propiedades anestésicas y el dolor durante la anestesia con inyección a chorro sin aguja: un ensayo clínico aleatorizado. Rev Ciênc Oral Aplic. 2019;27:e20180195.
- Hayward SC, Landorf KB, Redmond AC. Ice reduces needle-stick pain associated with a digital nerve block of the hallux. Foot. 2006;16(3):145-8. DOI: 10.1016/j.foot.2006.04.001.