10.20986/revesppod.2025.1720/2024
ORIGINAL
Correlation between plantar fascia thickness, foot function, and physical activity level in men with plantar fasciopathy
Correlación entre el grosor de la fascia plantar, la función del pie y el nivel de actividad física en hombres con fasciopatía plantar
Rubén Montes Salas1
Ramón Mahillo Durán1
José Manuel Castillo López1
1Departamento de Podología. Universidad de Sevilla, España
Abstract
Objectives: This study aims to investigate the relationship between plantar fascia thickness and clinical and anthropometric variables specific to men diagnosed with plantar fasciitis.
Patients and methods: A total of 44 feet from male patients were randomly selected. Plantar fascia thickness was measured using ultrasound imaging and correlated with pain intensity, functional impairment, height, age, weight, plantar fascia biconvexity, disease duration, recurrence of plantar fasciitis, and daily physical activity levels.
Results: The average plantar fascia thickness was 5.97 ± 1.08 mm. Significant predictors included the absence of prior treatment, shorter height, higher Foot Function Index (FFI) scores, and shorter disease duration. Increased thickness was observed in men with biconvex fascia morphology and athletes, likely due to the impact of physical activity.
Conclusions: This study highlights the multifactorial relationship between plantar fascia thickness and clinical variables in men. These findings support the development of more targeted diagnostic and therapeutic strategies.
Keywords: Plantar fasciitis, plantar fascia thickness, ultrasound, physical activity, foot, men
Resumen
Objetivos: Este estudio tiene como objetivo investigar la relación entre el grosor de la fascia plantar y las múltiples variables clínicas y antropométricas específicas de los hombres diagnosticados con fascitis plantar.
Pacientes y métodos: Se seleccionaron aleatoriamente 44 pies de pacientes masculinos. El grosor de la fascia plantar se midió mediante ecografía, analizando su correlación con la intensidad del dolor, el deterioro funcional, la altura, la edad, el peso, la biconvexidad de la fascia plantar, la duración de la enfermedad, la recurrencia de la fascitis plantar y los niveles de actividad física.
Resultados: El grosor promedio de la fascia plantar fue de 5.97 ± 1.08 mm. Los predictores significativos de un mayor grosor fueron la ausencia de tratamiento previo, menor altura, puntuaciones más altas en el Índice de Función del Pie (FFI) y una menor duración de la enfermedad. Además, el grosor aumentó en hombres con morfología biconvexa de la fascia y en deportistas, posiblemente por el impacto de la actividad física.
Conclusiones: Este estudio aporta información sobre los factores asociados al grosor de la fascia plantar en hombres, destacando la importancia de la evaluación clínica y ecográfica para desarrollar estrategias de manejo más específicas y efectivas.
Palabras clave: Fascitis plantar, grosor de la fascia plantar, ecografía, actividad física, pie, hombre
Corresponding author
Rubén Montes Salas
rubmonsal@alum.us.es
Received: 12-01-2024
Accepted: 22-01-2025
Introduction
Plantar fasciitis is one of the most common causes of heel pain(1), with characteristics that vary between men and women. Reviewing the literature, few previous studies have focused on the differences in this pathology based on sex and its biomechanical and functional particularities. Factors such as differences in connective tissue density, hormonal variations, and sex-specific physical activity patterns could significantly influence the progression of this condition.
It is estimated that around 10 % of people will experience plantar fasciitis at some point in their lives. The incidence of this condition increases with age, being more frequent between 40 and 60 years. However, there is no clear consensus on whether it affects one sex more than the other(2), although some studies suggest a female-to-male predominance of 2:1(1,3)in the prevalence of the disease. These data underscore the importance of plantar fasciitis as a prevalent condition that significantly impacts the quality of life of those affected.
The pain associated with plantar fasciitis is often reproduced by palpation of the inferomedial tubercle of the calcaneus, which corresponds to the insertion site of the plantar fascia. Additionally, passive dorsiflexion of the foot and toes can exacerbate the characteristic pain of this condition. In this context, the Windlass test, also known as the Jack test, is often positive. This maneuver is considered positive when it elicits pain, reinforcing the clinical diagnosis of plantar fasciitis(4).
It has been studied that plantar fasciitis is caused by degeneration of the plantar fascia due to repetitive microtears from trauma or overuse, rather than a primary inflammatory reaction5. Therefore, the term plantar fasciosis and, more recently, plantar fasciopathy (PF) has been coined in the literature. The exact cause of PF remains unknown, although it is believed to be multifactorial, with abnormal biomechanics and delayed collagen healing in the fascia as potential contributors(6).
PF is associated with multiple risk factors. High-impact physical activities, such as long-distance running, ballet, or aerobic dance, increase the likelihood of developing this condition by generating greater pressure on the heel and adjacent tissues. Similarly, biomechanical abnormalities of the foot, such as flat feet, high arches, or an improper gait pattern, affect weight distribution, increasing tension on the plantar fascia. Overweight and obesity are significant factors, as excess body weight places additional load on the fascia. Additionally, occupations that require prolonged standing or walking, especially on hard surfaces, also increase the risk.
Finally, the use of inadequate footwear, such as shoes without proper arch support, can contribute to the development of the condition(2). Most patients seek treatment within the first year, and in most cases, pain resolves within the first year. Multiple treatments have been proposed in the medical literature, and most specialists opt to start with conservative treatment, which is effective in 70-80 % of cases. The most widely used approaches are physical therapy, orthotics, gastrocnemius stretching, and corticosteroid injections(7).
Studies have shown similar accuracy and efficacy of musculoskeletal ultrasound in the morphological evaluation and diagnosis of plantar fasciitis compared to magnetic resonance imaging(8) and even better according to other references9. Ultrasound is generally preferred due to certain advantages over MRI, such as its non-invasive nature, lower cost, and better patient tolerance. Ultrasound has reported thickening of the plantar fascia, tissue abnormalities, hypoechoic changes, perifascial fluid accumulation, and subcalcaneal bone spurs(8,9).
It appears that healthy men and women have similar plantar fascia thickness. However, as PF develops, men tend to develop thicker plantar fascias than women, which could have implications for the treatment chosen by the therapist(10).
In patients with plantar fasciitis, ultrasound may reveal, in some cases, mild intrafascial or perifascial hyperemia. However, in most cases, no significant increase in soft tissue vascularization is observed when routine Doppler ultrasound is used. Therefore, a positive Doppler signal should not be considered indispensable for establishing the diagnosis of this pathology. Rather, such a signal can be a complementary tool to personalize and optimize the therapeutic plan based on the individual characteristics of each patient(11).
Sex differences in the clinical manifestation and progression of PF have been poorly explored. Previous studies have identified that men may present greater fascial thickness and different biomechanical patterns compared to women. The objective of this work focuses on understanding these male-specific differences, with an emphasis on how anthropometric, functional, and physical activity variables contribute to the clinical characteristics of PF in men.
Patients and methods
The present study is a transverse case series of patients with PF.
Study population
To be included in the study, patients had to be men over 18 years of age. Patients also had to present symptoms consistent with PF and a plantar fascia thickness greater than 4 millimeters(12), measured by ultrasound in addition to agreeing to participate in the study.
Exclusion criteria included having systemic diseases or non-podiatric morpho-functional alterations that could affect the ankle and foot and lead to significant clinical discrepancies in the lower limbs, limb length discrepancies, or evident clinical scoliosis, having received any treatment (medical, orthopedic, and/or invasive) on the foot in the last three months, PF associated with another condition such as nerve entrapment, and difficulties on the part of the patient in understanding the instructions to be followed during treatment.
Used variables
All patients underwent a clinical evaluation and an ultrasound evaluation. The clinical evaluation was based on a visual analog scale (VAS) (13) (0-10) and the Foot Function Index (FFI) (14,15), which assesses function on a scale of 0 to 100. Subjects were also classified as sedentary, active, or athletes based on their daily physical activity, as well as whether it was the first time the disease appeared, a recurrence, or chronic(16). Sex, weight, and height were also evaluated, as well as the presence of vascularization in the plantar fascia visualized with ultrasound at the time of the initial evaluation and the biconvex17 or flattened shape of the plantar fascia (Figure 1).
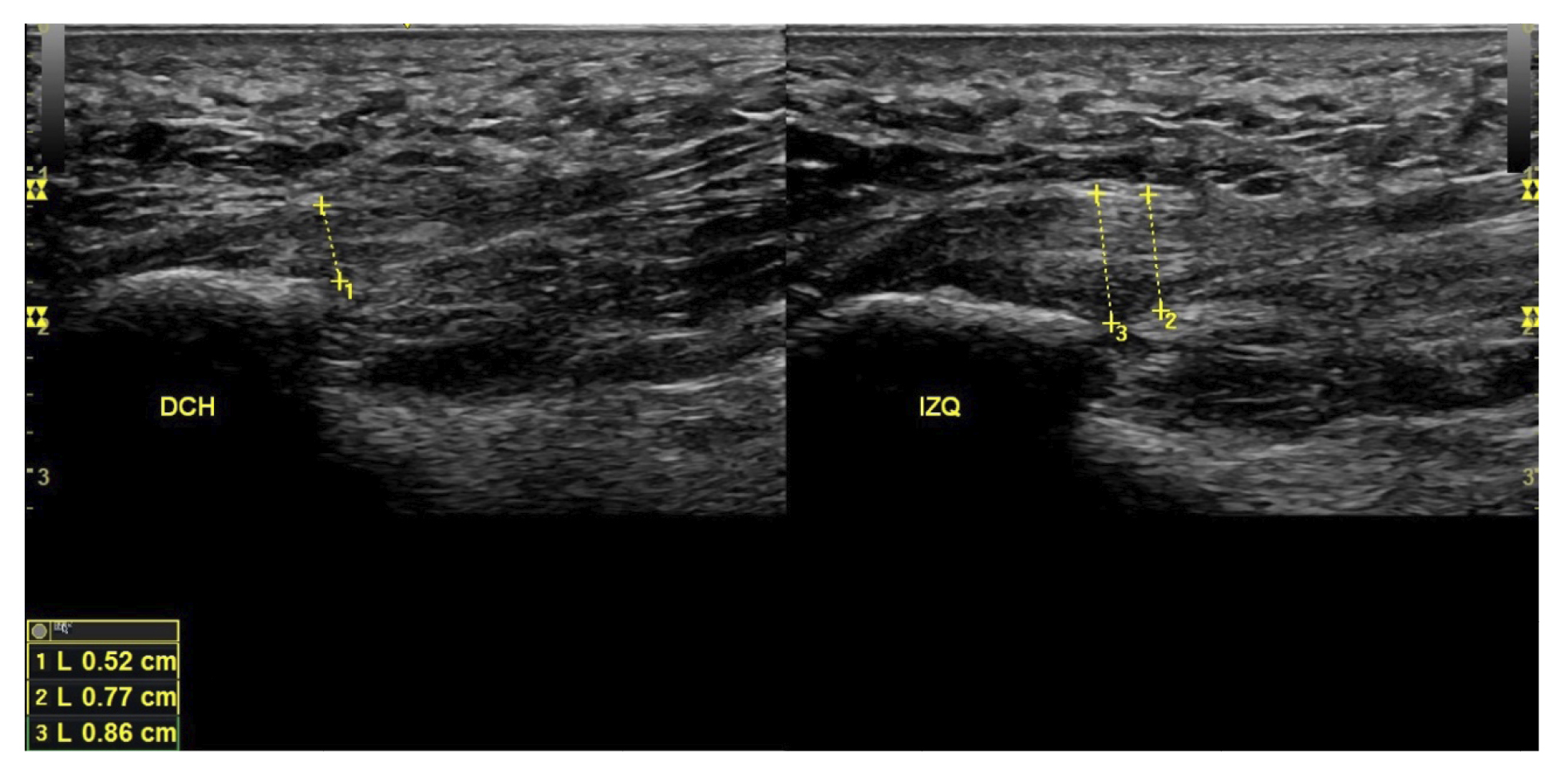
Figure 1. Plantar fascia with normal morphology on the left and biconvex plantar fascia on the right.
All patients had experienced the classic symptoms of PF, including pain when taking the first steps after waking up or after sitting for a long time. Patients felt pain upon palpation of the proximal plantar fascia and reported that the pain worsened as the day progressed. The diagnosis was established based on symptoms and confirmed by ultrasound using high-resolution equipment (Alpinion Ecube 9, ALPINION MEDICAL SYSTEMS Co., Ltd., Republic of Korea) with a 6-12 MHz linear transducer (Figures 2 and 3).
Figure 2. Researcher with the linear probe for measuring plantar fascia thickness.
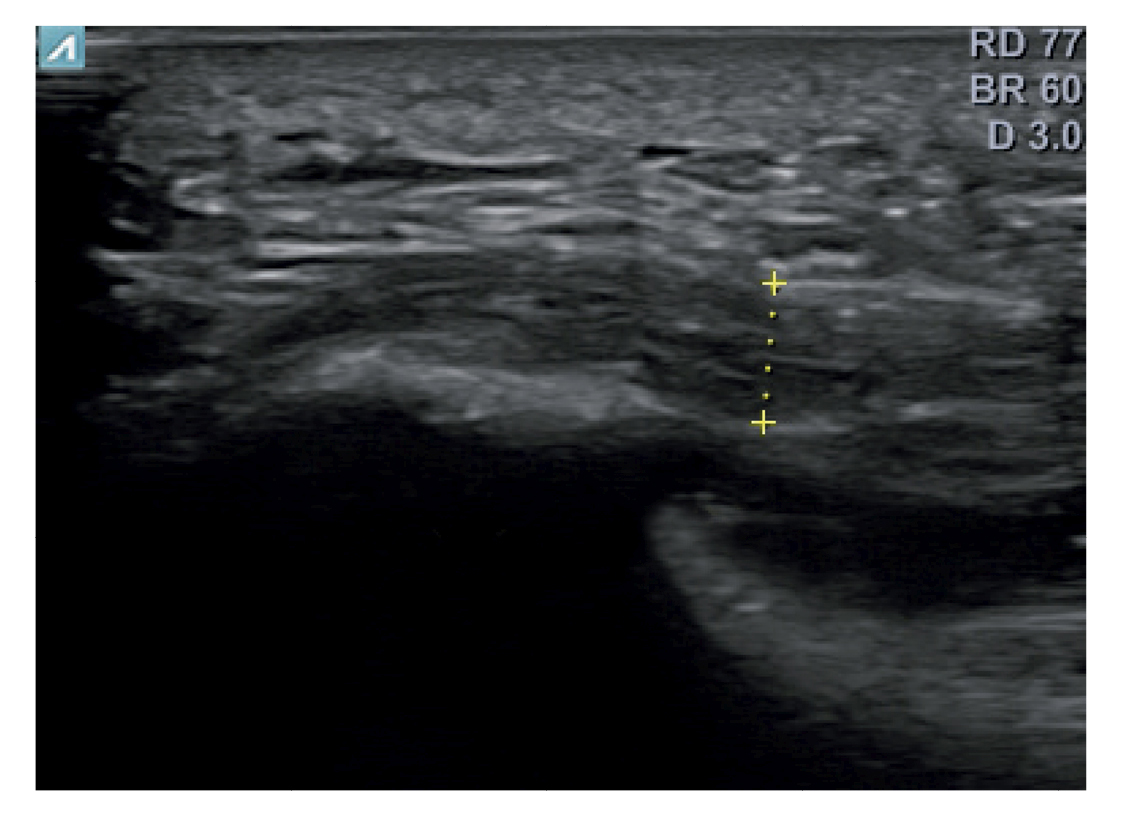
Figure 3. Area of measurement of plantar fascia thickness. The dotted line corresponds to the thickness measurement.
Statistical analysis
A descriptive analysis was performed for all quantitative and qualitative data. The normality of the variables was assessed using the Shapiro-Wilk test, with the variables following a normal distribution (p > 0.05) except for the previous treatment variable (p < 0.05) and body mass (p < 0.05). A regression analysis was performed relating the thickness of the plantar fascia measured by ultrasound with the other variables analyzed in the study to estimate the coefficients of the linear equation. p < 0.05 was considered statistically significant. Statistical analysis was performed using the IBM SPSS Statistics 25 package at a 95 % confidence level.
Results
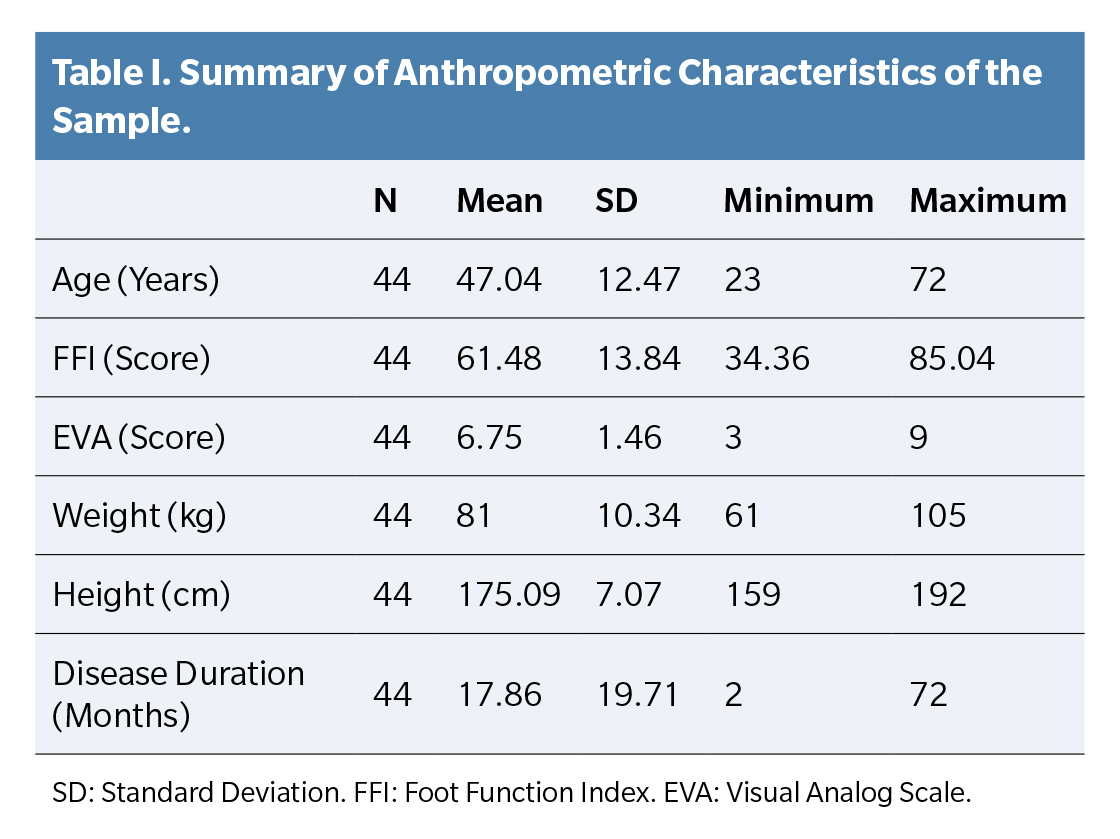
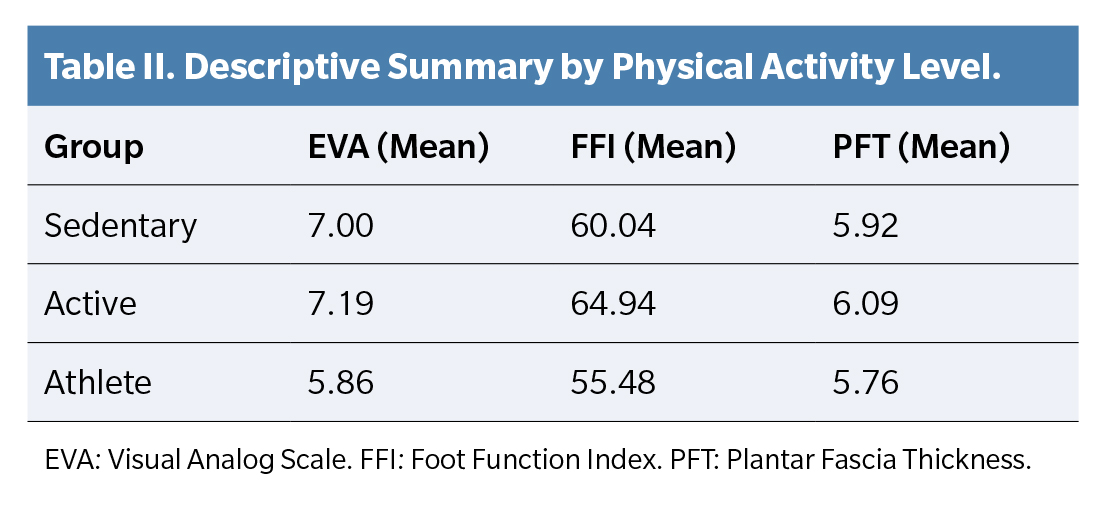
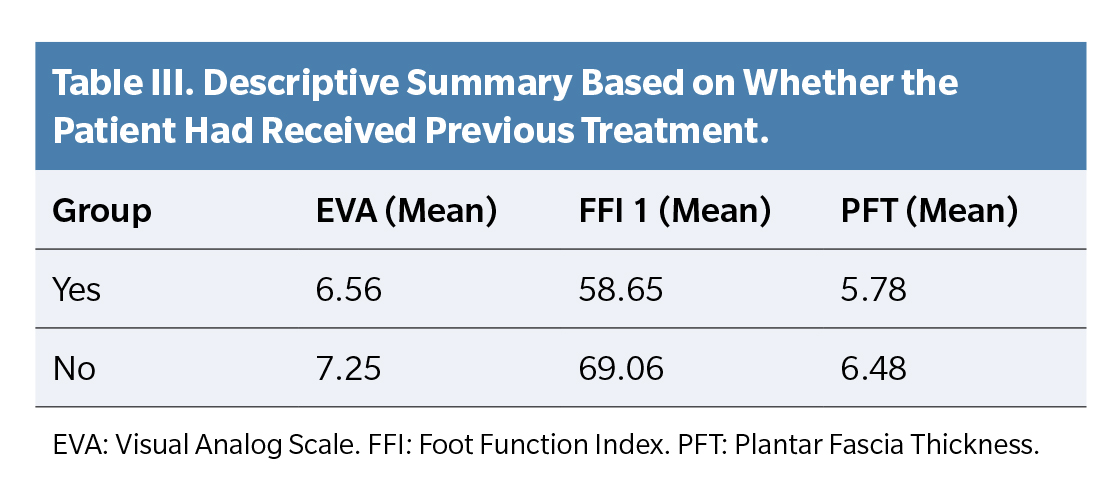
Total population was 44 patiens and the mean age of the patients was 47.05 ± 12.34 years. The mean score on the VAS scale was 6.75 ± 1.45. The mean function score on the FFI scale was 61.49 ± 13.69. The mean thickness of the plantar fascia was 5.97 ± 1.08. The mean body weight was 81 ± 10.35 kilograms, and the height was 175.09 ± 7.07 centimeters. In 15 subjects, the disease appeared for the first time, in 13 it was a recurrence, and in 16 it was considered chronic. Four subjects were sedentary, 26 were active, and 14 were athletes. The mean duration of the disease in months was 9.513 ± 6.58. Thirty-two patients had received previous treatment, and 12 had not. Nine presented biconvexity of the plantar fascia, and 35 did not (Tables 1, 2 and 3).
In the multiple linear regression analysis, a coefficient of determination R2 = 0.517 was obtained, indicating that the model explains 51.7 % of the variability in plantar fascia thickness. The predictors with statistical significance for greater plantar fascia thickness were, in order of relative importance: having received previous treatment (0.25), patient height in centimeters (0.23), foot function index measured with the FFI scale (0.21), duration of the disease in months (0.12), and, to a lesser extent, perceived pain according to the VAS scale (0.04).
The remaining variables analyzed did not show statistical significance in this model. These findings highlight the combined influence of clinical and anthropometric factors on the variability of fascial thickness. Specifically, the history of previous treatment and patient height emerged as the most relevant predictors, while perceived pain showed limited influence (Figure 4).
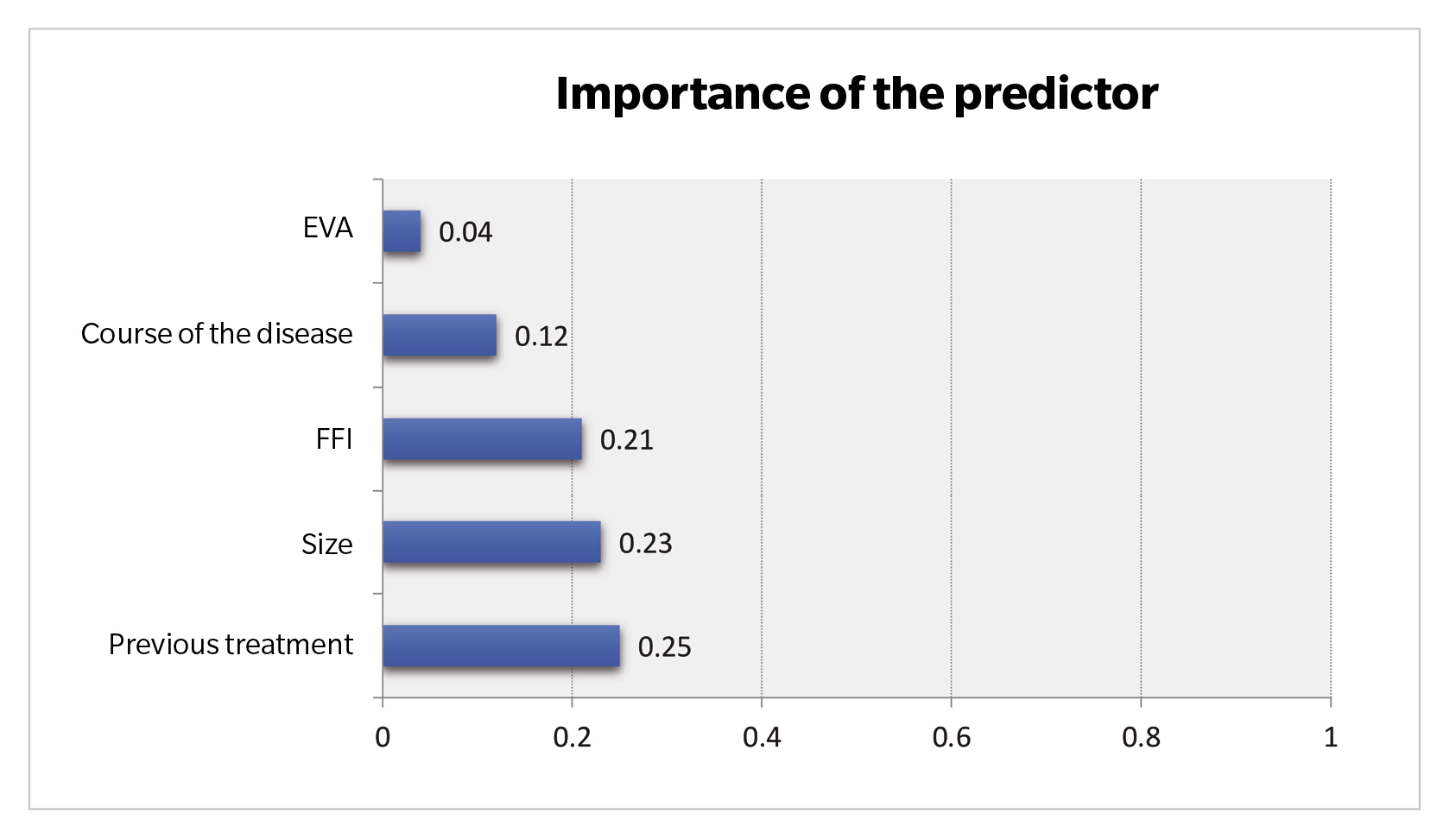
Figure 4. Predictor importance. VAS: Visual Analog Scale. FFI: Foot Function Index.
Discussion
The main objective of this study was to analyze the factors influencing plantar fascia thickness in patients with fasciopathy, specifically evaluating the impact of clinical and anthropometric variables such as previous treatment, height, FFI, disease duration, pain measured with the VAS scale, body mass, and biconvexity of the plantar fascia. The main results show that plantar fascia thickness is significantly associated with a history of previous treatment and patient height, followed by FFI and disease duration.
Prognostic factors in PF are frequently analyzed to provide information on the extent to which patients will benefit from different treatment modalities. Thickening of the plantar fascia is of particular interest, as it is a prominent and frequent manifestation of PF and can be quantitatively assessed.
In this descriptive study, the mean thickness of the plantar fascia in men with PF was 5.97 ± 1.08 mm, and the significant predictors of greater fascial thickness included not having received previous treatment, shorter height, a high score on the FFI scale, and a short duration of the disease.
In healthy individuals, plantar fascia thickness is closely correlated with age, height, weight, body mass index, and walking activity in the general population, and our descriptive study conducted in men diagnosed with PF shows some differences(19), such as greater fascial thickness in shorter individuals. Plantar fascia thickness has been positively associated with greater body height. In our study, this variable shows a negative correlation(20).
Having received previous treatment showed a positive correlation with lesser fascia thickness. Similarly, in our study, as plantar fascia thickness increased, patients experienced more pain. Changes in plantar fascia thickness serve as a valid objective measure to evaluate the efficacy of new or existing treatment protocols, and in general, the greater the fascia thickness, the more pain patients experience(21). The efficacy of clinical treatments in plantar fasciopathy can be measured by evaluating plantar fascia thickness.
Additionally, as plantar fascia thickness increased, patients also showed greater dysfunction, as indicated by higher scores on the FFI scale. This relationship has been previously studied by other authors, with conflicting conclusions in various studies(22,23).
In our study, greater plantar fascia thickness measured by ultrasound was associated with a shorter duration of the disease. That is, with a shorter duration of the disease, the thickness of the PF was greater. However, no literature was found to compare these data with other scientific studies.
Biconvexity of the PF is a condition that has rarely been studied, in which the structure presents an oval appearance. In our study, patients whose fascias were classified as biconvex had greater PF thickness. This finding suggests that biconvexity may be associated with structural changes in the fascia that accompany the progression of plantar fasciopathy.
In our study, patients were classified as sedentary, active, or athletes based on their self-perception. Athlete patients with the disease had greater plantar fascia thickness, a relationship that has been studied in the unaffected population, reaching the same conclusion20, although there is literature that does not show a relationship(24). More studies on this topic are needed, both in affected and unaffected populations.
Patients included in the study were categorized based on whether they presented a first episode, a recurrence, or a chronic condition of the disease. However, no significant correlations were identified in this classification. It should be noted that the definition of chronic heel pain varies widely in the literature, being considered chronic in some studies after one month, in others after three months, and in some cases after six months of duration(25). In our study, patients were classified as chronic when they had a symptom duration of more than six months. Additionally, no significant relationship was found between the presence of vascularization in plantar fasciopathy, observed by ultrasound at the initial evaluation, and fascia thickness in men.
The present study has several limitations. Firstly, this analysis focused exclusively on male patients diagnosed according to the previously described criteria. The difference in plantar fascia thickness between asymptomatic men and women has been the subject of analysis in the literature, highlighting that, according to Pascual Huerta, men present greater thickness, with a mean difference of 0.42 (26) and similar according to other authors(19,27). The presence or absence of a subcalcaneal spur was not considered in our descriptive study on male subjects. The relationship between the subcalcaneal spur and heel pain has been confirmed by multiple meta-analyses. However, a subpopulation of individuals with spurs is completely asymptomatic(28). The sample size of our study is small, and the precision of the correlation performed is low, highlighting the importance of conducting additional research with larger samples of the population affected by plantar fasciitis. By expanding the sample to a more diverse population, we will be able to more accurately assess whether the findings and conclusions of our study are generalizable to the general population. Additionally, it will be crucial to investigate possible differences in the presentation of plantar fasciitis between men and women, which could have important implications for the diagnosis and treatment of the disease.
Subsequent studies could include comparative analyses between groups of men and women to determine if there are disparities in the prevalence, severity, or response to treatment of plantar fasciitis. These analyses will help identify possible sex-specific risk factors and develop more personalized and effective treatment approaches. Furthermore, it may be important to consider the inclusion of more demographic and clinical variables in future studies to gain a more comprehensive understanding of the factors influencing the development and progression of plantar fasciopathy.
In conclusion, this study identified the main factors associated with plantar fascia thickness in male patients with PF. The results show that a history of previous treatment and height are the most relevant predictors, followed by FFI and disease duration, while perceived pain according to the VAS scale and other variables such as body mass and biconvexity had limited influence. These findings underscore the importance of considering clinical and anthropometric factors to understand variations in plantar fascia thickness and guide diagnostic and therapeutic interventions. Additionally, the data obtained reinforce the usefulness of combining clinical and ultrasound tools to assess the impact of different variables on this condition. Future research should focus on validating these results in larger cohorts and exploring specific interventions to optimize clinical outcomes in patients with PF.
Ethics declaration and consent to participate
Ethical approval was granted by University Hospital Universitario de Nuestra Señora de Valme Research Ethics Committee under protocol No. 2093-N-21. The ethical and human criteria established in the Declaration of Helsinki18 were followed. Informed and signed consent was obtained from all study participants.
Availability of data and materials
The datasets used and analyzed during the study are available from the corresponding author upon reasonable request.
Author contributions
Study conception and design: RMS, RMD.
Data collection: RMS, RMD.
Analysis and interpretation of results: RMD, JMCL.
Drafting, writing, and preparation of the manuscript: RMS, JMCL.
Final review: JMCL.
Conflicts of interest
None declared.
Funding
None declared.
References
- McNally EG, Shetty S. Plantar fascia: imaging diagnosis and guided treatment. Semin Musculoskelet Radiol. 2010;14(3):334-43. DOI: 10.1055/s-0030-1254522.
- Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25(5):303-10. DOI: 10.1177/107110070402500505.
- Rasenberg N, Bierma-Zeinstra SMA, Bindels PJ, van Middelkoop M, van der Lei J. Incidence, prevalence, and management of plantar heel pain: a retrospective cohort study in Dutch primary care. Br J Gen Pract. 2019;69(688):E801-8. DOI: 10.3399/bjgp19X706061.
- Alshami AM, Babri AS, Souvlis T, Coppieters MW. Biomechanical evaluation of two clinical tests for plantar heel pain: the dorsiflexion-eversion test for tarsal tunnel syndrome and the windlass test for plantar fasciitis. Foot Ankle Int. 2007;28(4):499-505.
- Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93(3):234-7.
- Lee WCC, Wong WY, Kung E, Leung AKL. Effectiveness of adjustable dorsiflexion night splint in combination with accommodative foot orthosis on plantar fasciitis. J Rehabil Res Dev. 2012;49(10):1557-64.
- Rhim HC, Kwon J, Park J, Borg-Stein J, Tenforde AS. A systematic review of systematic reviews on the epidemiology, evaluation, and treatment of plantar fasciitis. Life. 2021;11(12):1287.
- Sabir N, Demirlenk S, Yagci B, Karabulut N, Cubukcu S. Clinical utility of sonography in diagnosing plantar fasciitis. J Ultrasound Med. 2005;24(8):1041-8.
- Radwan A, Wyland M, Applequist L, Bolowsky E, Klingensmith H, Virag I. Ultrasonography, an effective tool in diagnosing plantar fasciitis: a systematic review of diagnostic trials. Int J Sports Phys Ther. 2016;11(5):663-71.
- Granado MJ, Lohman EB, Daher NS, Gordon KE. Effect of Gender, Toe Extension Position, and Plantar Fasciitis on Plantar Fascia Thickness. Foot Ankle Int. 2019;40(4):439-46. DOI: 10.1177/1071100718811631.
- McMillan AM, Landorf KB, Gregg JM, De Luca J, Cotchett MP, Menz HB. Hyperemia in plantar fasciitis determined by power Doppler ultrasound. J Orthop Sports Phys Ther. 2013;43(12):875-80. DOI: 10.2519/jospt.2013.4810.
- McMillan AM, Landorf KB, Barrett JT, Menz HB, Bird AR. Diagnostic imaging for chronic plantar heel pain: A systematic review and meta-analysis. J Foot Ankle Res. 2009;2(1):1-11. DOI: 10.1186/1757-1146-2-32.
- Thong ISK, Jensen MP, Miró J, Tan G. The validity of pain intensity measures: what do the NRS, VAS, VRS, and FPS-R measure? Scand J Pain. 2018;18(1):99-107. DOI: 10.1515/sjpain-2018-0012.
- Paez-Moguer J, Budiman-Mak E, Cuesta-Vargas AI. Cross-cultural adaptation and validation of the Foot Function Index to Spanish. Foot Ankle Surg 2014;20(1):34-9. DOI: 10.1016/j.fas.2013.09.005.
- Budiman-Mak E, Conrad KJ, Roach KE. The Foot Function Index: a measure of foot pain and disability. J Clin Epidemiol. 1991;44(6):561-70. DOI: 10.1016/0895-4356(91)90220-4.
- Pardo y Camps F. Eficacia de la infiltración de Plasma Rico en Plaquetas (PRP) en pacientes diagnosticados del Síndrome de la Fascia Plantar (SFP) desde el punto de vista clínico y functional [Tesis de master]. Universidad Complutense de Madrid]; 2016.
- Fleischer AE, Albright RH, Crews RT, Kelil T, Wrobel JS. Prognostic Value of Diagnostic Sonography in Patients With Plantar Fasciitis. J Ultrasound Med. 2015;34(10):1729-35. DOI: 10.7863/ultra.15.14.10062.
- World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-4. DOI: 10.1001/jama.2013.281053.
- Narindra L, Herinirina N, Rakotonirina H, Andrianah G, Ranoharison H, Randriamboavonjy R, et al. Thickness of the Plantar Fascia in Asymptomatic Subjects. J Med Ultrasound. 2019;27(3):121-3. DOI: 10.4103/JMU.JMU_72_18.
- Abul K, Ozer D, Sakizlioglu SS, Buyuk AF, Kaygusuz MA. Detection of normal plantar fascia thickness in adults via the ultrasonographic method. J Am Podiatr Med Assoc. 2015;105(1):8-13. DOI: 10.7547/8750-7315-105.1.8.
- Mahowald S, Legge BS, Grady JF. The correlation between plantar fascia thickness and symptoms of plantar fasciitis. J Am Podiatr Med Assoc. 2011;101(5):385-9.
- Gamba C, Sala-Pujals A, Perez-Prieto D, Ares-Vidal J, Solano-Lopez A, Gonzalez-Lucena G, et al. Relationship of Plantar Fascia Thickness and Preoperative Pain, Function, and Quality of Life in Recalcitrant Plantar Fasciitis. Foot Ankle Int. 2018;39(8):930-4. DOI: 10.1177/1071100718772041.
- Mahowald S, Legge BS, Grady JF. The correlation between plantar fascia thickness and symptoms of plantar fasciitis. J Am Podiatr Med Assoc. 2011;101(5):385-9. DOI: 10.7547/1010385.
- Uzel M, Cetinus E, Ekerbicer HC, Karaoguz A. The influence of athletic activity on the plantar fascia in healthy young adults. J Clin Ultrasound. 2006;34(1):17-21. DOI: 10.1002/jcu.20178.
- Koc TA, Bise CG, Neville C, Carreira D, Martin RL, McDonough CM. Heel Pain - Plantar Fasciitis: Revision 2023. J Orthop Sports Phys Ther. 2023;53(12):CPG1-39. DOI: 10.2519/jospt.2023.0303.
- Pascual Huerta J, Alarcónn García JM. Effect of gender, age and anthropometric variables on plantar fascia thickness at different locations in asymptomatic subjects. Eur J Radiol. 2007;62(3):449-53.
- Gadalla N, Kichouh M, Boulet C, Machiels F, De Mey J, De Maeseneer M. Sonographic evaluation of the plantar fascia in asymptomatic subjects. JBR-BTR. 2014;97(5):271-3. DOI: 10.5334/jbr-btr.1326.
- Kirkpatrick J, Yassaie O, Mirjalili SA. The plantar calcaneal spur: a review of anatomy, histology, etiology and key associations. J Anat. 2017;230(6):743-51. DOI: 10.1111/joa.12607.