10.20986/revesppod.2025.1711/2024
ORIGINAL
Treatment of plantar fascitis with intratissue percutaneous electrolysis. Systematic review and metaanalisis
Tratamiento de la fasciopatía plantar con electrólisis percutánea intratisular. Revisión sistemática y metanálisis
Ana M.ª Rayo Pérez1
Rafael Rayo Martín1
Francisco Javier Rodríguez Castillo1
Raquel García de la Peña1
1Departamento de Podología. Universidad de Sevilla, España
Abstract
Introduction: Plantar fasciitis is one of the leading causes of heel pain, accounting for between 11 % and 15 % of all foot-related pain consultations. In this context, over one million people seek medical attention for heel pain each year, with up to 80% of these cases diagnosed as plantar fasciitis.
Material and methods: A comprehensive search was conducted across major scientific databases, following a standardized systematic review and meta-analysis strategy. Studies evaluating the effects of Percutaneous Intratissue Electrolysis (EPI) on patients with plantar fasciitis were included, comparing its outcomes with other therapeutic interventions or placeb.
Results: The systematic review and meta-analysis suggest that EPI is an effective therapeutic option for plantar fasciitis, showing significant benefits in pain reduction and functional improvement in the medium term. Patients treated with EPI reported being asymptomatic at the end of the treatment, highlighting its effectiveness compared to conventional interventions. Furthermore, its efficacy appears to be comparable to that observed in the treatment of tendinopathies, such as patellar tendinitis, which share similar histopathological features with plantar fasciitis.
Conclusion: EPI emerges as an effective and safe alternative for the treatment of plantar fasciitis, contributing to pain reduction and functional improvement in affected patients. These findings support its use in clinical practice as a valid option for managing this common foot condition.
Keywords: Plantar fasciitis, percutaneous intratissue electrolysis, invasive treatment, fasciopathy
Resumen
Introducción: La fasciopatía plantar es una de las principales causas de dolor en la región del talón, siendo responsable de entre el 11 y el 15 % de las consultas relacionadas con dolor en el pie. En este contexto, más de un millón de personas buscan atención médica por dolor en el talón cada año, y hasta el 80 % de estos casos son diagnosticados con fasciopatía plantar.
Material y método: Se llevó a cabo una búsqueda exhaustiva en las principales bases de datos científicas, siguiendo una estrategia estandarizada de revisión sistemática y metanálisis. Se incluyeron estudios que evaluaron el efecto de la electrólisis percutánea intratisular (EPI) en pacientes con fasciopatía plantar, comparando sus resultados con otras intervenciones terapéuticas o placebo.
Resultados: La revisión sistemática y el metanálisis sugieren que la EPI es una opción terapéutica efectiva para la fasciopatía plantar, mostrando beneficios significativos en la reducción del dolor y la mejora funcional a medio plazo. Los pacientes tratados con EPI reportaron ser asintomáticos al finalizar el tratamiento, destacando su efectividad en comparación con intervenciones convencionales. Además, se observó que su eficacia puede ser comparable a la observada en el tratamiento de tendinopatías como la tendinitis rotuliana, que comparten características histopatológicas similares con la fasciopatía plantar.
Conclusión: La EPI se presenta como una alternativa eficaz y segura para el tratamiento de la fasciopatía plantar, contribuyendo a la reducción del dolor y a la mejora funcional de los pacientes afectados. Estos hallazgos respaldan su uso en la práctica clínica como una opción válida para manejar esta condición común del pie.
Palabras clave: Fasciopatía plantar, electrólisis percutánea intratisular, tratamiento invasivo, fasciopatía
Corresponding author
ana M.ª Rayo Pérez
anarayo43@gmail.com
Received: 09-10-2024
Accepted: 08-12-2024
Introduction
Plantar fasciopathy (PF) is one of the most prevalent foot conditions, representing between 11 % and 15 % of professional consultations related to pain in this region. It is estimated that more than one million people seek medical attention annually for heel pain, with 80 % of them diagnosed with plantar fasciopathy. It mainly affects individuals between 40 and 60 years old and is common in approximately 10 % of athlete runners(1,2,3).
This multifactorial condition can be classified according to anatomical and biomechanical factors. Anatomical factors include flat feet, cavus feet, obesity, and shortening of the posterior musculature, while biomechanical factors involve excessive pronation, limited ankle dorsiflexion, weakness of the plantar flexor musculature, and intrinsic foot weakness. Extrinsic factors such as barefoot walking, wearing inappropriate footwear, or hard surfaces also contribute to increased tension in the plantar fascia(4,5).
PF manifests as heel pain that occurs when weight-bearing after prolonged rest, exacerbating with prolonged standing or walking. Its diagnosis is mainly clinical, although imaging modalities such as ultrasound, considered the gold standard, help identify structural changes such as increased fascial thickness and rule out other differential diagnoses. Although initially associated with an inflammatory process, histological studies indicate that PF involves a chronic degenerative process—fasciosis— characterized by repeated microtrauma leading to tissue degeneration without active inflammation(3,4,5,6).
Conservative treatment is the initial option in PF, showing efficacy in 80 % of cases over 12 months. It includes plantar orthoses, orthotic wedges, and modified footwear, designed to support the longitudinal arch and reduce tension in the plantar fascia. Additionally, anti-inflammatory therapies—ultrasound, ice, rest—manual techniques, stretching of the triceps surae and plantar fascia, and functional taping for short-term pain relief are employed(5,6).
Among physical therapies, EPI stands out, a minimally invasive technique that uses galvanic current applied through an acupuncture needle. This procedure generates an electrochemical reaction that promotes controlled local inflammation, phagocytosis, and repair of damaged tissue(7,8,9).
EPI induces an electrolytic ablation of the degenerated tissue by causing changes in the pH of the treated area through the application of direct current in a saline environment. This triggers a chemical reaction that fragments collagen and degenerated myxoid substance. The technique is performed under ultrasound guidance, allowing for needle visualization and avoiding complications such as nerve or vascular injuries(8,9). The retrotracing technique is used, with 3 interventions per affected area. The established safety parameters are currents of 2 to 4 mA, 20 volts, and a duration of 4 seconds, ensuring a therapeutic effect without inducing adverse effects. During the application, ultrasound detects hyperechoic images generated by gas density, confirming the real-time effectiveness of electrolysis(9,10,11).
Several studies support EPI as a safe and effective therapeutic option for PF. Compared to traditional methods such as orthoses and stretching, EPI shows a faster resolution of pain and functional improvement in the medium term(12,13). Furthermore, its similarity with techniques used in tendinopathies (e.g., patellar tendinitis) strengthens its applicability in chronic degenerative conditions(7,8,9).
The primary endpoint of this article is to evaluate by means of metanalysis, the safety and efficacy profile of EPI in the treatment of plantar fasciopathy. Secondary endpoints include analyzing pain reduction in patients treated with EPI vs conventional treatments or placebo and determining the impact of EPI treatment on the functional improvement of the foot.
Material and methods
Study design
This study was conducted under the design of a systematic review with a subsequent meta-analysis. The methodology followed the guidelines of the PRISMA framework to ensure transparency and reproducibility in the data collection and analysis.
Bibliographic search
A comprehensive bibliographic search was conducted across the following specialized Health Sciences databases: PubMed, Cochrane Library, Dialnet, and Google Scholar. The keywords used in the search were: “Plantar Fasciitis,” “Fasciitis Plantaris,” “Heel Pain,” “Percutaneous Electrolysis,” “Intratissue Percutaneous Electrolysis,” and “EPI.”
- After establishing the keywords, various search strategies were formulated, leading to the following results: (“Plantar fascitis” OR “Fasciitis Plantaris”) AND (“Percutaneous Electrolysis” OR “Intratissue Percutaneous Electrolysis” OR “Electrolysis”),
- (“Plantar fascitis” OR “Fasciitis Plantaris” OR “Heel Pain”) AND (“Percutaneous Electrolysis” OR “Intratissue Percutaneous Electrolysis” OR “EPI” OR “Electrolysis”), and
- (“Plantar fascitis” OR “Fasciitis Plantaris” OR “Heel Pain”) AND (“Percutaneous Electrolysis” OR “Intratissue Percutaneous Electrolysis” OR “EPI” OR “Electrolysis”) AND (randomized controlled trial OR clinical trial OR “controlled study”).
Inclusion and exclusion criteria
Once the databases searchers were defined, the inclusion and exclusion criteria were established. Articles in Spanish and English published from 2014 through December 2024 were included in the study, including the following types: randomized clinical trials (RCTs), non-randomized clinical trials, quasi-experimental studies, and controlled studies where the study subjects were adult patients (≥ 18 years) diagnosed with plantar fasciopathy. Observational studies without a control group, animal studies, and clinical cases or case series were excluded. Additionally, studies with subjects having comorbidities affecting treatment—eg, rheumatoid arthritis—were excluded.
Study Selection
First, the principal investigator (RGP) conducted the bibliographic search following the previously established protocol and according to the PRISMA guidelines. Then, two independent reviewers (AMRP, FJRC) examined the titles and abstracts of the studies found to determine their relevance. Articles that passed the initial screening were evaluated in full text to verify that they met the inclusion criteria. Finally, in case of disagreement, a third reviewer made the final decision (Figure 1).
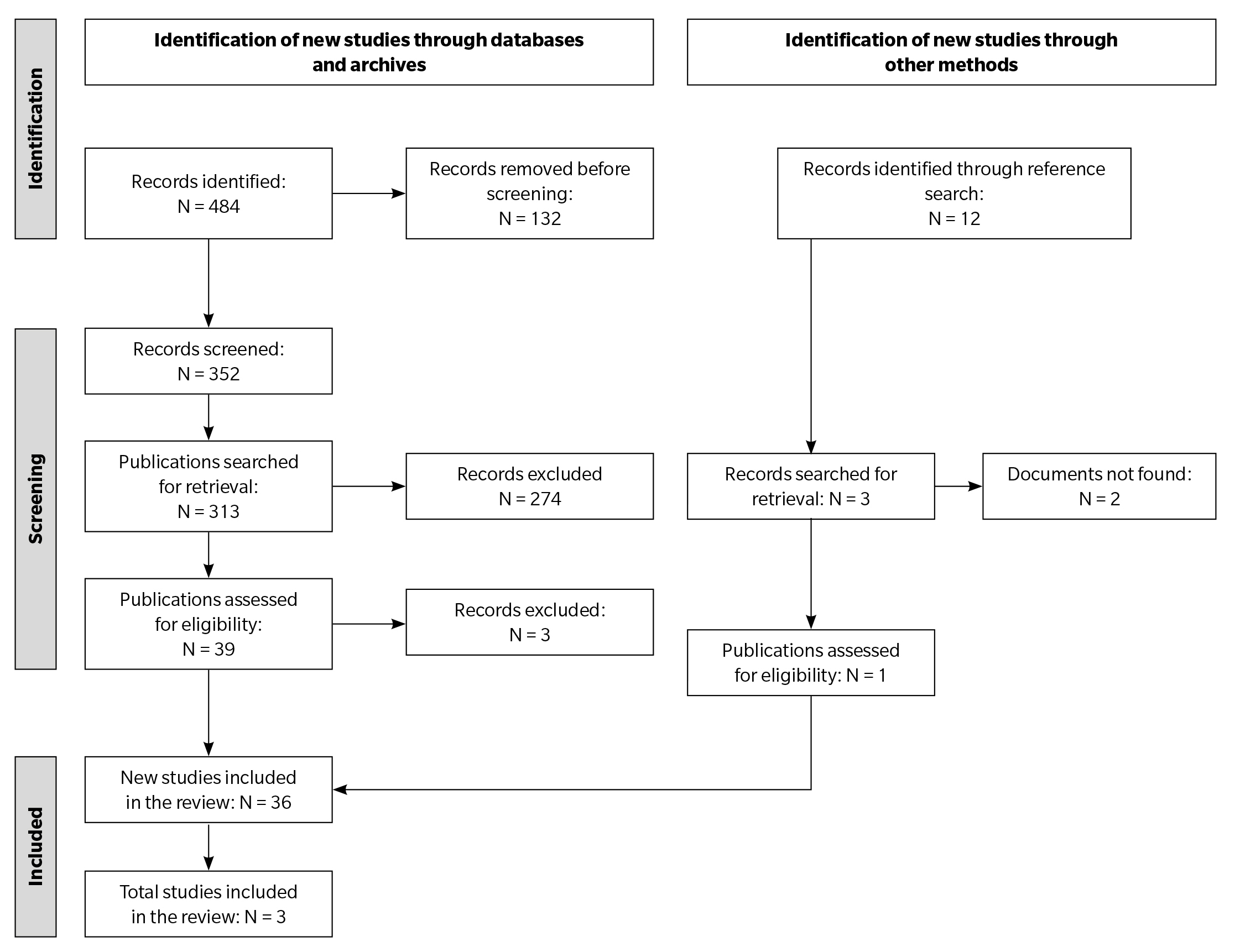
Figure 1. Flowchart.
Assessment of study quality
The methodological quality of the selected studies was assessed using appropriate tools: the Cochrane Risk of Bias Tool for randomized clinical trials and MINORS (Methodological Index for Non-Randomized Studies) for non-randomized studies.
Data extraction and analysis
A standardized data extraction form was designed, which included the following items:
- General information (authors, year, country, study type).
- Participant characteristics: age, gender, duration of plantar fasciopathy.
- Intervention details: type and protocol of EPI, number of sessions, duration of treatment.
- Comparator: type of treatment (placebo or active).
- Main outcomes: pain reduction, functional improvement, quality of life, adverse events.
- Follow-up: follow-up time, losses to follow-up.
Additionally, a meta-analysis was conducted using the Review Manager software version 5.4 (RevMan). Results were combined using random-effects models if significant heterogeneity was detected (assessed using the I² statistic). Weighted mean differences (WMD) were used for continuous outcomes (such as pain or functionality), and relative risks (RR) for dichotomous outcomes (adverse events).
The robustness of the results was evaluated by excluding low-quality studies or those with a high risk of bias. The heterogeneity among the studies was assessed using the I² statistic and the Cochran heterogeneity test (Q). Significant heterogeneity was considered if I² value > 50 %.
Results
A total of 484 studies were identified, 39 of which were selected after applying the inclusion and exclusion criteria. Subsequently, after conducting a critical reading and assessing the methodological quality of the studies, three articles were selected for inclusion in the systematic review and meta-analysis.
The detailed results of the quality assessment of the studies, as well as the results of the statistical analyses, are shown in Table 1.
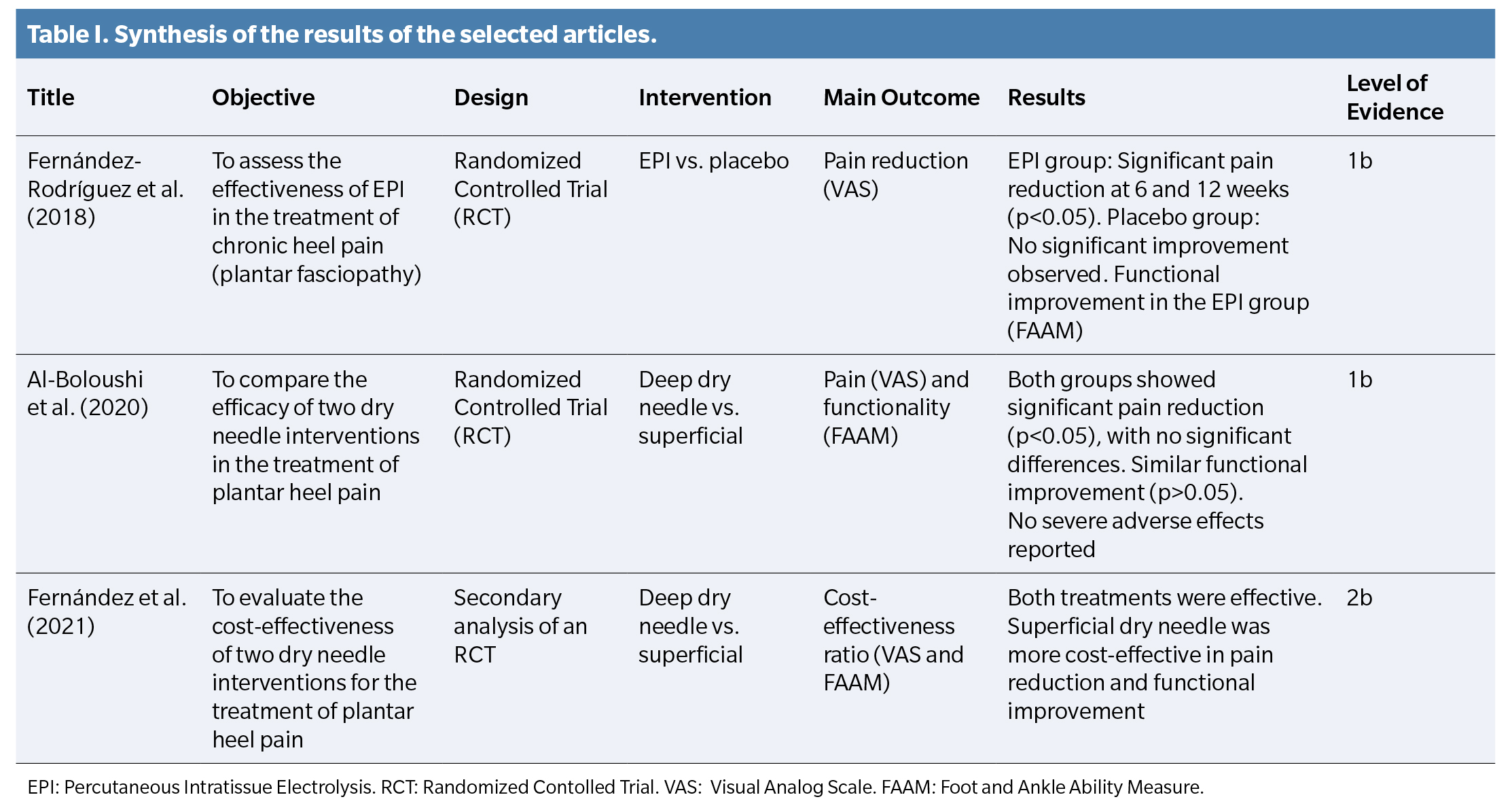
The risk of bias in the selected studies was evaluated using appropriate tools for randomized clinical trials. The results of the bias analysis for each of the articles are shown in Table 2. All studies presented a low risk of bias in most of the domains assessed. However, higher risks were identified in the areas of “blinding of participants” in the study by Al-Boloushi et al. (14) and “blinding of assessors” in the study by Fernández et al. (15).
The methodological quality of the selected studies was evaluated using the MINORS scale. The total score of the studies ranged between 18 and 21 points out of a maximum of 24, indicating a reasonably high methodological quality, though with some limitations, especially in studies that were not fully randomized.
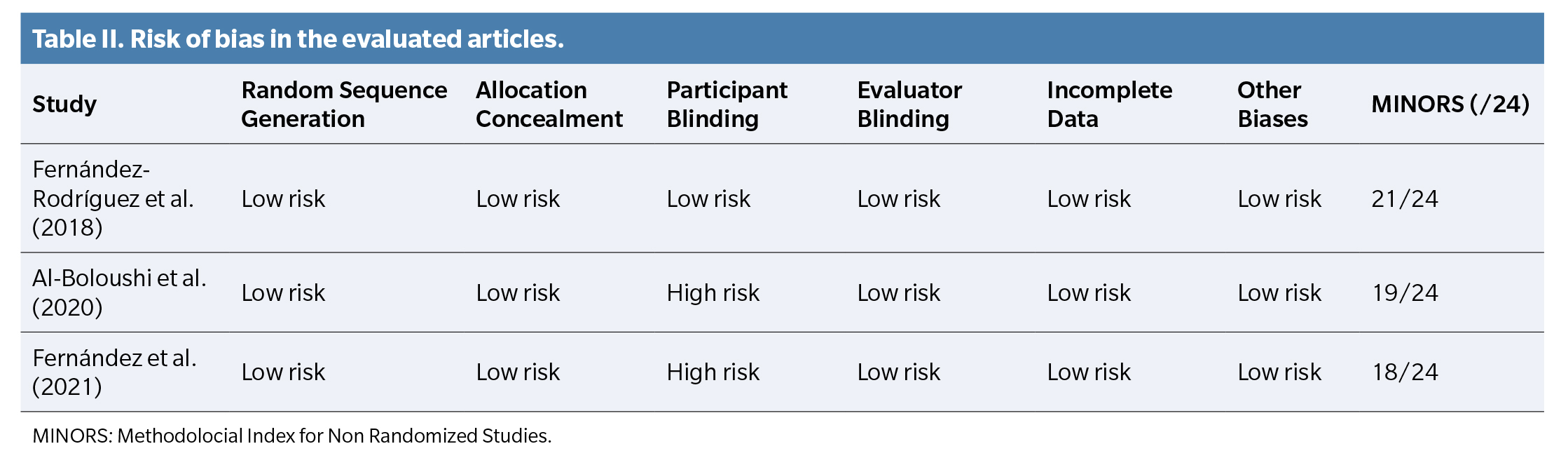
Regarding pain reduction, a weighted mean difference (WMD) analysis was conducted between the intervention and comparator groups. Figure 2 presents the individual results of the mean difference for pain reduction on the Visual Analog Scale (VAS). The study by Fernández-Rodríguez et al. (15) showed a mean reduction of 4.2 points in the EPI group compared to 1.3 points in the placebo group, while Al-Boloushi et al. (15,16)reported a reduction of 3.5 points in the EPI group compared to 3.2 points in the superficial dry needle group.
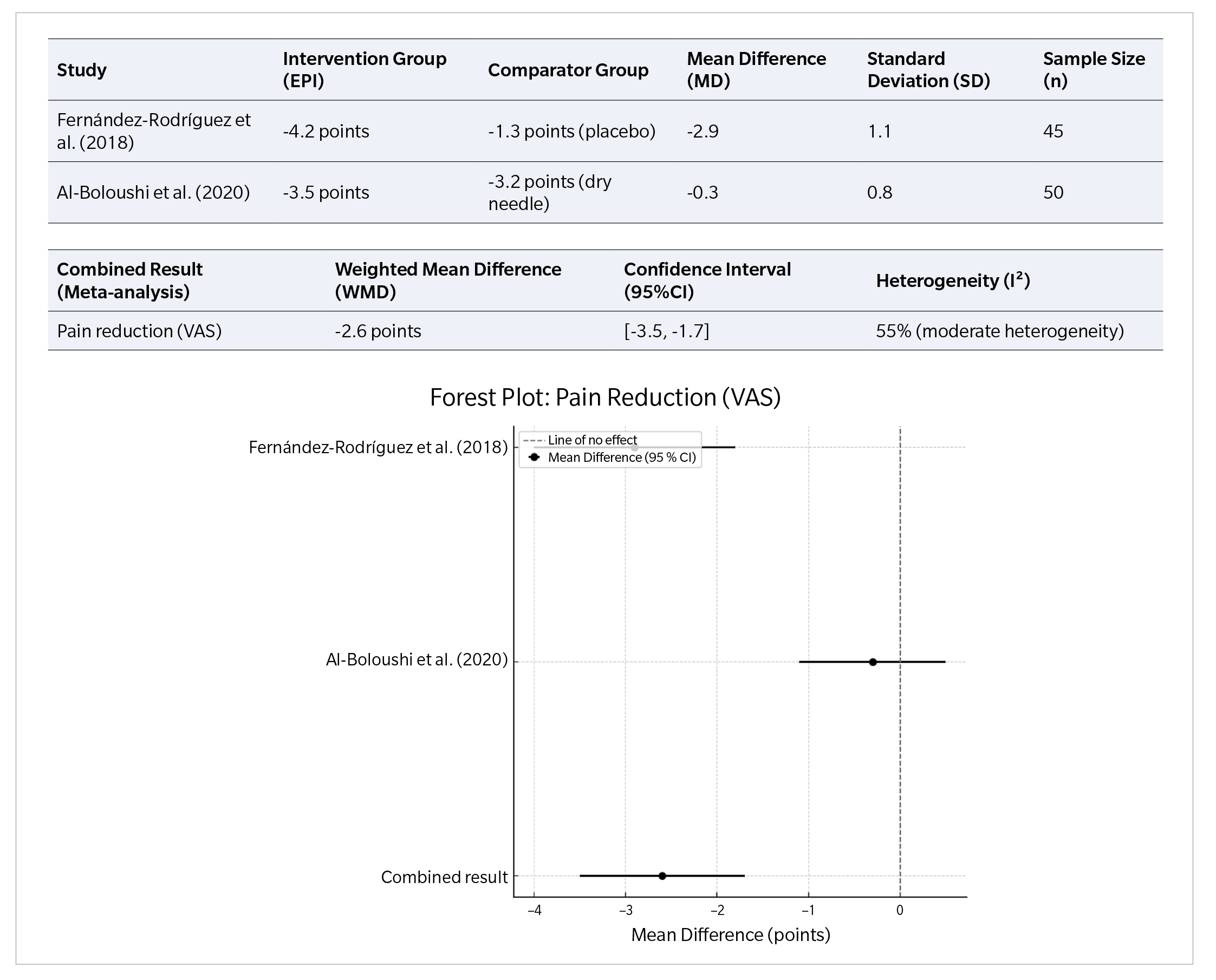
Figure 2. Pain reduction analysis on the visual analog scale (VAS).
The combined meta-analysis of the three studies (Figure 2) showed a WMD of -2.6 points on the VAS scale in favor of the EPI intervention compared to placebo or superficial dry needling. The results were statistically significant, with a confidence interval (95 %CI) between -3.5 and -1.7. However, moderate heterogeneity was detected between the studies (I² = 55 %), indicating that the variability in the results might be influenced by differences in intervention protocols and the characteristics of the studied populations.
Regarding functional improvement, changes in the Foot and Ankle Ability Measure (FAAM) were evaluated. Figure 3 presents the results of the mean difference between the intervention and comparator groups. Fernández-Rodríguez et al. reported a 30 % functional improvement in the EPI group compared to 10 % in the placebo group, while Al-Boloushi et al. found a 28 % improvement in the EPI group vs. 25 % in the superficial dry needle group.
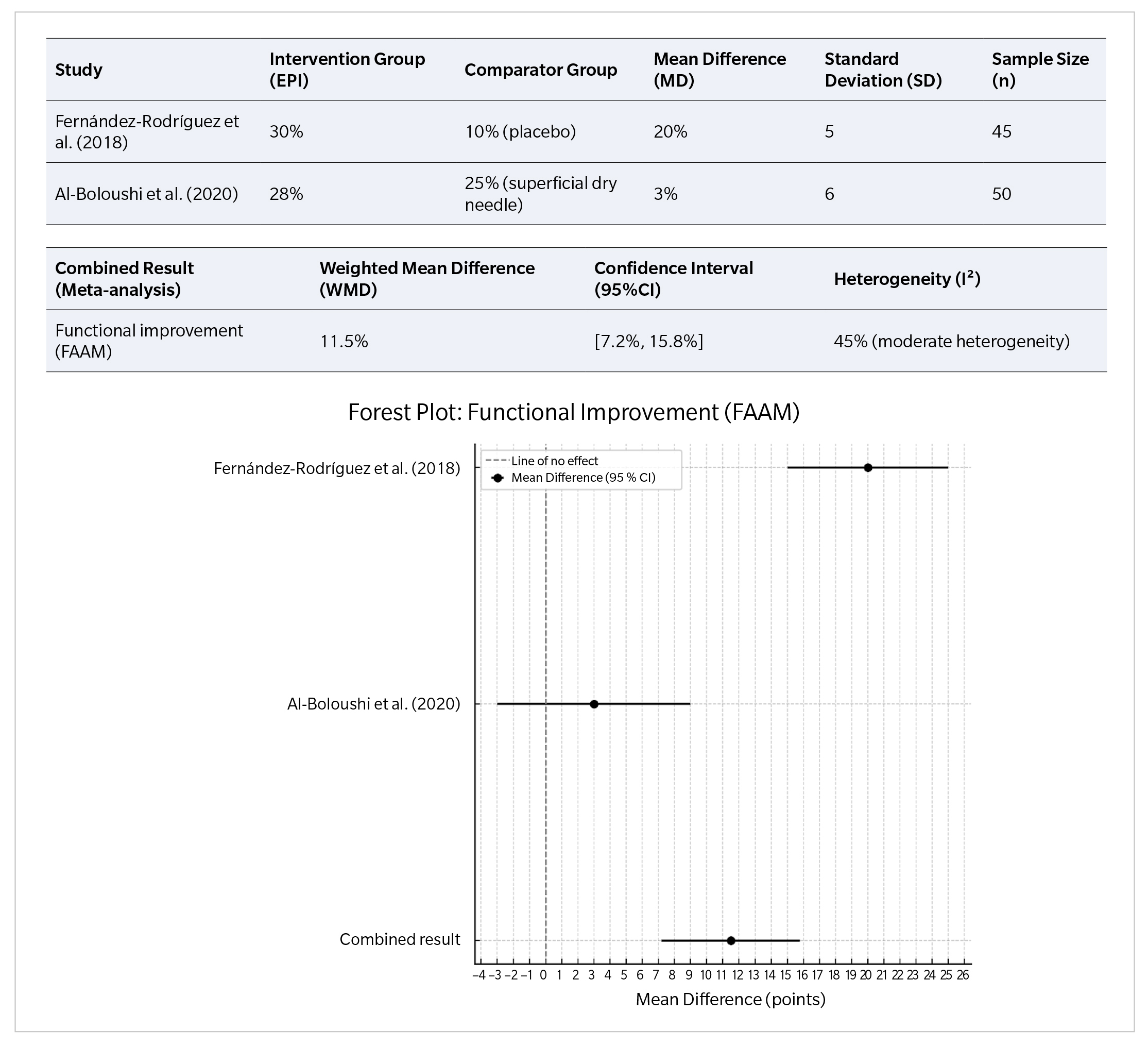
Figure 3. Functional Improvement Analysis by means of Foot and Ankle Ability Measure (FAAM).
The combined meta-analysis of the studies (Figure 3) showed a WMD in functional improvement of 11.5 % in favor of EPI vs placebo or superficial dry needling. The results were also statistically significant, with a 95%CI between 7.2 % and 15.8 %. The heterogeneity between the studies was moderate (I² = 45%), suggesting that factors such as the treatment protocol or patient characteristics may have influenced the results.
Discussion
In this study, a total of 484 articles were reviewed, 39 of which were initially selected based on the established inclusion and exclusion criteria. After a critical evaluation and analysis of the methodological quality, three studies were chosen for inclusion in the systematic review and meta-analysis. The selected studies showed reasonably high methodological quality, with MINORS scale scores ranging from 18 to 21 out of 24, and most presented a low risk of bias in key domains, although limitations related to the blinding of participants and assessors were identified.
In terms of the obtained results, the combined analysis indicated that EPI produced a significant reduction in pain, with a weighted mean difference of -2.6 points on the VAS vs placebo or superficial dry needling. Additionally, a significant functional improvement was observed, with a weighted mean difference of 11.5% on the Foot and Ankle Ability Measure (FAAM) in favor of EPI. However, of note, the moderate heterogeneity observed in both analyses (I² = 55 % for pain reduction and I² = 45 % for functional improvement) suggests that factors such as variations in intervention protocols and population characteristics could have influenced the results.
Following the line of our study, in 2018 and 2010, respectively, Iborra-Marcos et al.4 and Sánchez-Ibáñez et al. (12) showed clinical improvements in their studies regarding pain (VAS-P) or functionality (VAS-F) in the application of EPI for plantar fasciopathy. The first study, unlike the second, conducted a comparative study in which half of the 64 participants were treated with EPI, and the other half were administered a corticosteroid injection.
In both studies, EPI treatment was applied to the proximal insertion of the plantar fascia. In the first article, participants who were not athletes were included, some of whom had been diagnosed with plantar fasciopathy for 3 months, considering that this short period of time would positively influence a quicker recovery of the disease since it is treated before it progresses further. In the second study, the participant was a male athlete with plantar fasciopathy diagnosed with a one-year evolution, who had not been treated with conservative therapy previously(4,12).
An essential point included in the study by Iborra-Marcos et al (4) is the prior conservative treatment, as they mention the existence of participants who had received other treatments before the administration of EPI, suggesting that effective results in treating plantar fasciopathy do not necessarily depend exclusively on the application of the EPI treatment.
Both authors mention that the current intensity used in the first EPI session was 3 mA. Iborra-Marcos et al. state that an intensity of 3 mA is sufficient to induce angiogenesis and repair the tissues of the plantar fascia(4). Sánchez-Ibáñez et al. report in their study that (12) EPI sessions were administered, one every 5 days, with a treatment duration of 2 months from the first visit until the subject became asymptomatic. On the other hand, Iborra-Marcos et al.4 administered a 3 mA current for 5 seconds, repeating the treatment for 7 days, and then again, up to 10 sessions at weekly intervals as necessary. The mean number of sessions provided to the participants was 5.2, with one subject requiring only 3 sessions to become asymptomatic.(12).
Regarding the advantages, the time required to achieve symptom cessation for the above-mentioned conditions stands out. In the reviewed studies, the authors agree that EPI treatment for plantar fasciopathy and patellar tendinopathy is effective in the mid-term, being an excellent technique for addressing these conditions, as it shows optimal results in relatively short periods of time. Additionally, as an advantage over the use of EPI, it is highlighted that only two subjects presented adverse effects, specifically vasovagal episodes, as reported in the study by Iborra-Marcos et al., while in other studies, no subjects presented any adverse effects(4).
On the other hand, the authors mention as disadvantages the lack of a blinded group and the small number of subjects in the study samples. In 2015, Abat et al. indicated that EPI is contraindicated in subjects who are pregnant, have knee prostheses, osteosynthesis, heart disease, malignant tumors, or coagulopathy. Additionally, it is important to note the difficulty in conducting studies with a larger number of subjects due to the barrier that participants face in attending weekly EPI treatments13. Pain associated with the use of EPI is also considered, which is why Garrido et al. .(9), in 2019, and Iborra-Marcos et al. (4), in 2018, included subjects who were administered anesthesia before EPI application, in areas near the lesion. Finally, it must be considered that the combination of EPI with other treatments impacts the reliability of the studies when evaluating EPI as a first-choice treatment.
The main limitation corresponds to the primary endpoint of this review and meta-analysis, as the number of scientific articles published on the treatment of plantar fasciopathy using EPI is very limited. These studies have a small number of participants, which makes it more difficult to establish results and conclusions. In addition to the small number of studies that have applied EPI to subjects with plantar fasciopathy, it is important to note that the studies found include a small number of participants, which also limits the completeness of the results. On the other hand, the analyzed studies are longitudinal prospective studies that lack a control group, which negatively affects the reliability of the technique applied. Therefore, further research studies on the treatment of plantar fasciopathy through EPI therapy are necessary.
One of the main strengths of this study is that it is the first systematic review that includes a meta-analysis on pain reduction and functional improvement associated with EPI treatment in patients with plantar fasciopathy. Additionally, the rigorous selection of articles through well-defined inclusion and exclusion criteria was emphasized, along with the critical evaluation of the methodological quality of the included studies.
In conclusion, the studies included in this work show that EPI could be an effective intervention for reducing pain and improving functionality in subjects with plantar fasciopathy, compared to placebo or superficial dry needling treatments. EPI stands out for its ability to generate clinically significant pain reduction and improve patients’ quality of life. However, the risk of bias in some studies, especially the blinding of subjects, must be considered when interpreting the results.
Conflicts of interest
None declared.
Funding
None declared.
Authors’ contributions
Study conception and design: AMRP.
Data collection: AMRP.
Analysis and interpretation of results: RRM, FJRC, RGP.
Conception, drafting, and preparation of the initial draft: FJRC.
Final review: RGP.
References
- Cotchett M, Lennecke A, Medica VG, Whittaker GA, Bonanno DR. The association between pain catastrophising and kinesiophobia with pain and function in people with plantar heel pain. Foot (Edinb). 2017;32:8-14. DOI: 10.1016/j.foot.2017.03.003.
- Johnson RE, Haas K, Lindow K, Shields R. Plantar fasciitis: what is the diagnosis and treatment? Orthop Nurs. 2014;33(4):198-204. DOI: 10.1097/NOR.0000000000000063.
- Fernández-Rodríguez T, Fernández-Rolle Á, Truyols-Domínguez S, Benítez-Martínez JC, Casaña-Granell J. Prospective randomized trial of electrolysis for chronic plantar heel pain. Foot Ankle Int. 2018;39(9):1039-46. DOI: 10.1177/1071100718773998.
- Iborra-Marcos Á, Ramos-Álvarez JJ, Rodriguez-Fabián G, Del Castillo-González F, López-Román A, Polo-Portes C, et al. Intratissue percutaneous electrolysis vs corticosteroid infiltration for the treatment of plantar fasciosis. Foot Ankle Int. 2018;39(6):704-11. DOI: 10.1177/1071100718754421.
- Schwartz EN, Su J. Plantar fasciitis: a concise review. Perm J. 2014;18(1):e105-7. DOI: 10.7812/TPP/13-113.
- Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, et al. Heel pain-plantar fasciitis: revision 2014. J Orthop Sports Phys Ther. 2014;44(11):A1-33. DOI: 10.2519/jospt.2014.0303.
- Graham ME, Jawrani NT, Goel VK. Evaluating plantar fascia strain in hyperpronating cadaveric feet following an extra-osseous talotarsal stabilization procedure. J Foot Ankle Surg. 2011;50(6):682-6. DOI: 10.1053/j.jfas.2011.07.005.
- Sánchez-Ibáñez JM, Fernández ME. Ultrasound-guided EPI® technique and eccentric exercise, new treatment for Achilles and patellar tendinopathy focused on the region-specific of the tendon. Orthop Muscular Syst. 2015;4:1000200. DOI: 10.4172/2161-0533.1000200.
- Garrido V, Muñoz M, Ibáñez S. Effectiveness of electrolysis percutaneous intratissular (EPI®) in chronic insertional patellar tendinopathy. Trauma Fund MAPFRE. 2010;21:227-36.
- Sánchez-Ibáñez JM, Estévez M, Directores R, Ma D, Carmona P, Gil T. Evolución clínica en el tratamiento de la entesopatía rotuliana crónica mediante electro-estimulación percutánea ecodirigida. 2012;1-370.
- Sánchez-Ibáñez JM. Fisiopatología de la regeneración de los tejidos blandos. Madrid: McGraw Hill; 2005.
- Sánchez-Ibáñez J. Fasciopatía plantar: tratamiento regenerativo mediante electrólisis percutánea intratisular (EPI®). Rev Esp Podol Clin. 2010;2:22-9.
- Abat F, Vallés SL, Gelber PE, Polidori F, Stitik TP, García-Herreros S, et al. Mecanismos moleculares de reparación mediante la técnica Electrólisis Percutánea Intratisular en la tendinosis rotuliana. Rev Esp Cir Ortop Traumatol. 2014;58(4):201-5. DOI: 10.1016/j.recot.2014.01.002.
- Al-Boloushi Z, Gómez-Trullén EM, Arian M, Fernández D, Herrero P, Bellosta-López P. Comparing two dry needling interventions for plantar heel pain: a randomised controlled trial. BMJ Open. 2020;10(8):e036245. DOI: 10.1136/bmjopen-2020-038033.
- Fernández D, Al-Boloushi Z, Bellosta-López P, Herrero P, Gómez M, Calvo S. Cost-effectiveness of two dry needling interventions for plantar heel pain: a secondary analysis of an RCT. Int J Environ Res Public Health. 2021;18(4):1777. DOI: 10.3390/ijerph18041777.
- Al-Boloushi Z, Gómez-Trullén EM, Bellosta-López P, López-Royo MP, Fernández D, Herrero P. Comparing two dry needling interventions for plantar heel pain: a protocol for a randomized controlled trial. J Orthop Surg Res. 2019;14(1):31. DOI: 10.1186/s13018-019-1066-4.