10.20986/revesppod.2025.1728/2025
CLINICAL NOTE
Molluscum pendulum on the foot. Clincal case
Molluscum pendulum en el pie. Caso clínico
Joao Miguel Costa Martiniano1
Rafael Rayo Rosadom2
Rafael Rayo Martín2
Sandra Sánchez-Morilla2
Raquel García de la Peña2
Ana M.ª Rayo Pérez2
1Escola Superior de Saúde da Cruz Vermelha Portuguesa. Portugal
2Departamento de Podología. Universidad de Sevilla, España
Abstract
Molluscum pendulum, also known as acrochordon or pedunculated fibroma, is a benign fibroepithelial tumor that predominantly devel- ops in areas of friction, such as the neck, armpits, and genital region. Its relationship with metabolic disorders, including obesity and insulin resistance, has been widely documented. However, its appearance on the plantar surface is extremely rare, which makes the documentation of this type of cases relevant. Surgical excision is the treatment of choice for large lesions, while less invasive options, such as cryotherapy and CO2 laser therapy, are commonly used in small lesions. It is presented a clinical case of a 56-year-old male patient with a pedun- culated fibroma in the plantar region. The intervention consisted of surgical excision with an advancement flap under local anesthesia, with the aim of achieving complete elimination of the lesion and minimizing biomechanical alterations in gait. The histopathological study confirmed the diagnosis of molluscum pendulum, showing epidermal acanthosis, hyperkeratosis and an increase in the amount of fibroblasts and collagen in the dermis. Postoperative follow-up was carried out for two years to evaluate the patient‘s clinical evolution and possible recurrence of the lesion.
Keywords: Molluscum pendulum, acrochordon, pedunculated fibroma, dermatological surgery, plantar lesión
Resumen
El molluscum pendulum, también conocido como acrocordón o fibroma pediculado, es un tumor fibroepitelial benigno que se desarrolla predominantemente en zonas de fricción, tales como el cuello, las axilas y la región genital. Su relación con trastornos metabólicos, incluyendo la obesidad y la resistencia a la insulina, ha sido ampliamente documentada. No obstante, su aparición en la superficie plantar es extremadamente infrecuente, lo que hace relevante la documentación de este tipo de casos. La escisión quirúrgica es el tratamiento de elección para lesiones de gran tamaño, mientras que opciones menos invasivas, como la crioterapia y la terapia con láser de CO2, se emplean habitualmente en lesiones pequeñas. Se presenta un caso clínico de un paciente masculino de 56 años con un fibroma pediculado en la región plantar. La intervención consistió en la escisión quirúrgica con colgajo de avance bajo anestesia local, con el objetivo de lograr la eliminación completa de la lesión y minimizar las alteraciones biomecánicas en la marcha. El estudio histopatológico confirmó el diagnóstico de molluscum pendulum, evidenciando acantosis epidérmica, hiperqueratosis y un incremento en la cantidad de fibroblastos y colágeno en la dermis. Se llevó a cabo un seguimiento postoperatorio durante 1 año para evaluar la evolución clínica del paciente y la posible recurrencia de la lesión.
Palabras clave: Molluscum pendulum, acrocordón, fibroma pediculado, cirugía dermatológica, lesión plantar
Correspondence
Ana M.ª Rayo Pérez
anarayo43@gmail.com
Received: 02-03-2025
Accepted: 05-05-2025
Introduction
Molluscum pendulum, also known as acrochordon or skin tag, is a benign skin lesion with a higher prevalence in women than in men, especially in individuals older than 40 years. These lesions typically develop in areas of skin folds or regions subject to friction, such as the neck, armpits, eyelids, submammary region, and inguinal region(1,2).. It’s estimated that up to 46 % of adults may develop skin tags at some point in their lives, although incidence rates vary depending on the population studied and the diagnostic methods employed.
Their appearance has been linked to metabolic disorders, particularly obesity and type 2 diabetes mellitus, as well as hormonal and mechanical changes characteristic of pregnancy. The possible pathophysiological connection between these conditions and the formation of skin tags could be due to insulin resistance and increased epidermal growth factors, such as insulin-like growth factor type 1 (IGF-1), which have been implicated in cell proliferation and the development of benign skin lesions(1,3,4).
From a clinical perspective, skin tags initially present as soft papules ranging from 1 to 5 mm in diameter, which can increase in size to several centimeters in advanced stages. Their coloration varies from skin-colored to darker shades, depending on vascular supply and possible previous trauma. Their characteristic pendulous mobility is due to the presence of a narrow stalk connecting them to the underlying skin. Although generally asymptomatic, they can become painful if they undergo torsion, inflammation, or secondary ulceration(3,4,5).
The diagnosis of skin tags is primarily clinical, based on visual inspection and palpation. Their typical presentation includes soft, mobile, and pedunculated lesions, which are mostly asymptomatic. However, in cases of atypical presentation, unusual morphology, or an excessive number of lesions, a biopsy is recommended to rule out differential diagnoses, such as intradermal nevi, squamous papillomas, pedunculated seborrheic keratosis, and malignant lesions like pedunculated basal cell carcinoma or amelanotic melanoma(6,7).
Given their benign nature and the absence of symptoms in most cases, treatment is usually sought for cosmetic reasons or due to discomfort from friction and mechanical irritation. Therapeutic options include cryotherapy with liquid nitrogen, CO? laser ablation, electrocautery, and excision with scissors or scalpel. The choice of treatment depends on factors such as lesion size and location, patient preferences, and the treating physician’s experience(8,9).. Additionally, recent studies suggest a possible association between skin tags and insulin resistance, which could justify a comprehensive approach in patients with metabolic risk factors, including the evaluation of glycemic and lipid profiles in individuals with a high lesion burden(10).
The main objective of this paper is to describe a clinical case of molluscum pendulum located in the plantar region, emphasizing its atypical presentation and the associated diagnostic and therapeutic challenges. As secondary objectives, we aim to review the available therapeutic strategies and evaluate their efficacy in the treatment of large lesions.
Case report
In September 2023, a 56-year-old man presented for consultation due to the presence of a large dermal lesion on the plantar surface of his right foot. The patient reported that the lesion had been present for approximately 3 years, with an onset after a laceration sustained while bathing in a lake. The initial wound, approximately 2 cm in diameter, healed spontaneously without medical intervention, evolving through secondary intention healing.
The patient had no relevant medical history. He denied chronic illnesses, diabetes, dyslipidemias, or a family history of dermatological diseases. He had no known allergies and was not on chronic medication.
During the clinical evaluation, a well-demarcated, nodular mass measuring 4 cm × 4.5 cm was observed in the metatarsal region, connected to the second intermetatarsal space by a pedicle. The lesion showed no tenderness to palpation or evident inflammatory signs. Given its dimensions and morphological characteristics, a scheduled surgical excision was decided for December 2023 under local anesthesia.
A preoperative ultrasound was performed, which showed a well-demarcated, hyperechoic dermal mass, with no involvement of deep structures. Additionally, preoperative blood tests with a metabolic profile (fasting glucose, HbA1c, lipid profile) were requested, and the results were normal. No prior biopsy was performed given the typical morphology of the lesion and the absence of clinical or sonographic alarm signs.
The surgical procedure consisted of complete resection of the lesion, followed by closure using an advancement flap, designed considering the size of the lesion, local skin tension, and biomechanical implications in the weight-bearing area, with the aim of minimizing postoperative complications.
A regional block of the posterior tibial and superficial peroneal nerve was performed with 2% mepivacaine (10 mL). Conscious sedation with 2 mg IV midazolam was administered. Ischemia was achieved with a pneumatic tourniquet at the distal third of the leg, with a pressure of 250 mmHg.
Complete excision of the lesion was performed at the pedicle level, with ligation of the vascularization using absorbable 4/0 suture. Hemostasis was reinforced with low-intensity monopolar electrosurgery (Figure 1).
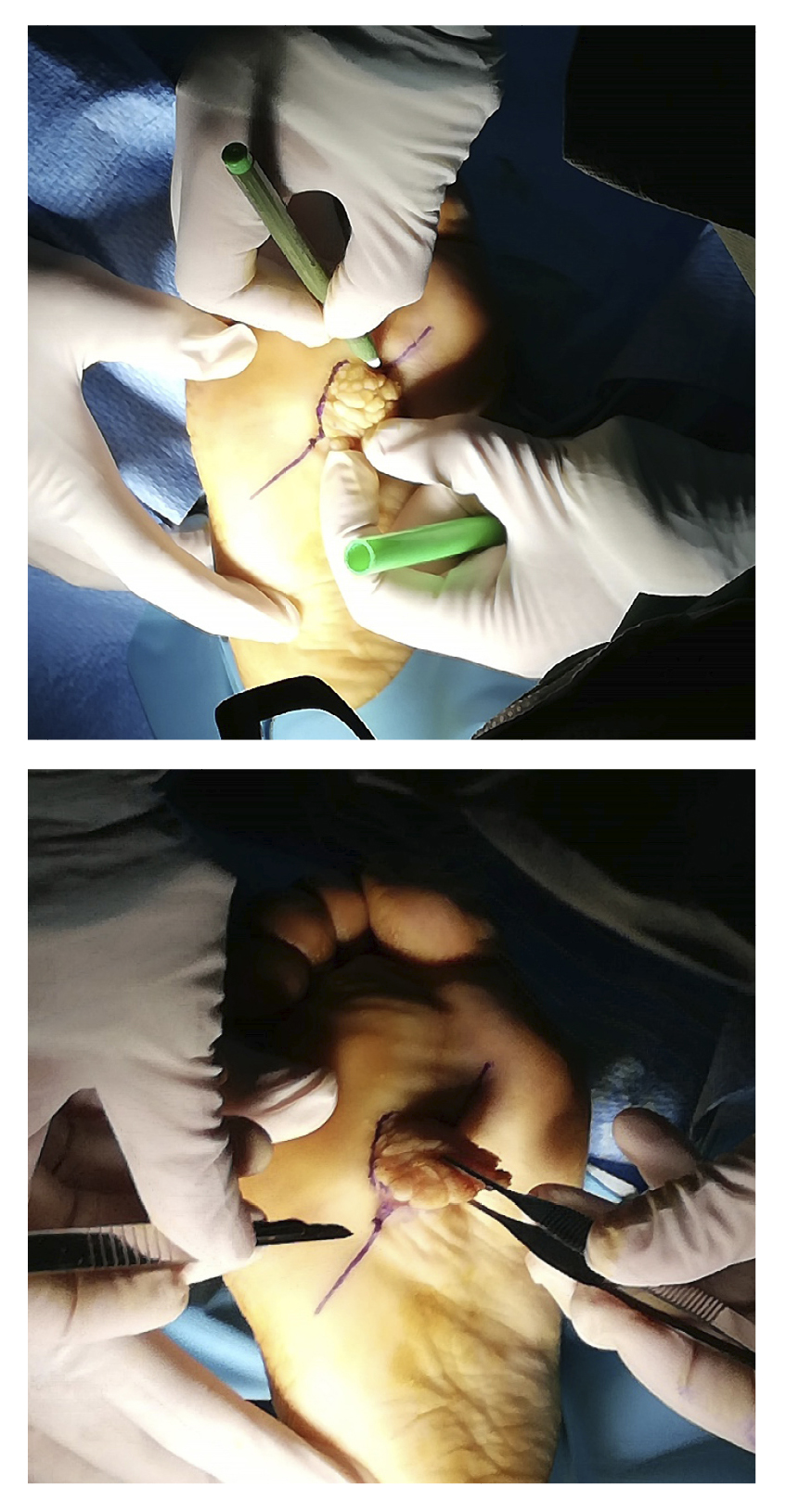
Figure 1. Intraoperative images.
Dissection was performed layer by layer with special caution to avoid damage to adjacent structures. The lesion was excised at the pedicle level, ensuring ligation of the vascular supply to prevent bleeding and recurrence. Subsequently, primary closure of the area was performed with layered sutures (layered closure with Vicryl 3/0 for deep dermis and nylon 4/0 for skin), optimizing tissue stability and promoting adequate healing (Figure 2).

Figure 2. Intraoperative images.
The excised specimen was sent for histopathological study. Macroscopic examination reported a pedunculated nodular lesion measuring 4.5 cm × 4 cm, with a smooth surface, light brown color, consistent on cutting, without necrosis or hemorrhages. Microscopic findings included epidermal acanthosis, hyperkeratosis, mild papillomatosis, and proliferation of dermal fibroblasts with compact collagen fibers. The mass presented a moderate perivascular lymphocytic infiltrate consistent with the chronic progression of the lesion.
Postoperative management included analgesia with Paracetamol 1g every 8 hours for 7 days and antibiotic prophylaxis with Azithromycin 500mg every 24 hours for 3 days. Dressings were changed every 72 hours for the first 10 days, using aqueous chlorhexidine, a hydrocolloid dressing, and a protective bandage. Suture removal was performed on day 15, and the use of a rigid Darco-type offloading brace was prescribed for 30 days to facilitate complete healing of the area. After brace removal, the use of padded orthopedic footwear was recommended to minimize pressure on the operated area and promote skin integrity.
The patient was definitively discharged 6 months after surgery, with no signs of recurrence or postoperative complications. Periodic follow-ups were conducted for one year, concluding in January 2025. These controls included clinical evaluations of skin integrity and foot function, ensuring optimal recovery without sequelae.
Discussion
Acrochordons, also known as soft fibromas or molluscum pendulum, represent one of the most frequent types of benign skin tumors, especially in middle-aged and elderly individuals. Although they typically localize in areas of friction such as the neck, armpits, or eyelids, their presentation in anatomically complex regions, such as the sole of the foot — as in the described case — is extremely unusual and poses a clinical challenge in both diagnosis and treatment.
In the present case, the plantar location dictated the choice of a surgical strategy that considered relevant biomechanical factors such as pressure and skin tension in the weight-bearing area of the foot. The use of an advancement flap allowed for adequate coverage of the defect, reducing the possibility of dehiscence, ulceration, and postoperative functional disorders. The literature supports the choice of surgical techniques adapted to anatomical location, especially in areas of high mobility or support, as observed in studies on reconstructive surgery in pendulous abdomen or large skin lesions of the lower limbs(10,11).
From an etiopathogenic standpoint, skin tags have been significantly associated with metabolic disorders, primarily obesity and insulin resistance. This relationship is supported by recent evidence highlighting a prominent role of insulin-like growth factor type 1 (IGF-1) in the proliferation of dermal fibroblasts, a key process in the formation of these lesions(12). In this case, the appearance of the lesion after minor trauma could be interpreted as a “Koebnerization” phenomenon, where a mechanical stimulus acts as a trigger in a metabolically predisposed terrain, a phenomenon also observed in other dermatoses.
The work of Hirt et al. (13). underscores how skin changes in obese patients go beyond simple adipose tissue accumulation, involving modifications in barrier function, microcirculation, and epidermal proliferation. This pathophysiological framework provides a comprehensive basis for understanding why certain individuals develop multiple or large skin tags. The relevance of a complete anamnesis and metabolic evaluation in these cases is, therefore, unquestionable. Unfortunately, in many case reports — including initially the present one — these antecedents are not exhaustively explored, which can limit a comprehensive view of the patient.
The histopathological study of the resected tissue, which revealed acanthosis, hyperkeratosis, and fibroblastic proliferation, aligns with the findings described by Saritas et al. (14). in their review of benign skin tumors, and by Higgins et al. (15), who emphasize that the histology of skin tags reflects typical changes associated with chronic lesions subjected to constant friction. Although the clinical diagnosis is usually evident, in atypical cases like this one — due to its location and size — biopsy is crucial to rule out other entities such as neurofibroma or even malignant lesions with a pedunculated morphology.
Another aspect of interest is postoperative management. The use of splints to avoid direct pressure on the operated area, as well as a dressing protocol every 48 hours with antiseptic solutions and hydrocolloid dressings, was effective in ensuring adequate healing. The need for standardized protocols in minor dermatological surgery has been highlighted by authors such as Graells et al. (16), who observed that proper postoperative planning can drastically reduce complications such as infections, partial necrosis, or suture dehiscence, especially in outpatient settings.
Regarding the surgical technique, it is relevant to note that direct ligation of the vascular pedicle was used instead of electrocoagulation, with the aim of preserving greater peripheral tissue viability. Although both techniques are valid, the choice must consider the anatomical environment, vascularization, and the presence of adjacent nervous structures. Bahce et al. (17) reported a similar case of a giant skin tag on the thigh successfully treated with excision and ligation, highlighting the importance of effective hemostatic control to avoid recurrences.
In terms of comparative literature, there is a notable lack of documented cases of plantar skin tags, which limits the possibility of establishing consistent clinical patterns or specific therapeutic protocols. However, studies such as those by Luba et al. (18) and Triwatcharikorn et al. (19) show that changes in the patient’s metabolic state — for example, after bariatric surgery — can lead to the regression or spontaneous disappearance of benign skin lesions, including skin tags. This emphasizes the need to address these lesions not only from a surgical approach but also from a systemic perspective, considering treatments that modify the patient’s hormonal and metabolic environment.
Finally, a limitation in the initial presentation of this case was the scarce photographic documentation of long-term follow-up. The inclusion of preoperative, intraoperative, and healing process images would provide added didactic and scientific value to the case, allowing for a better understanding of the results obtained and their temporal evolution. Image-based medicine constitutes a fundamental tool in surgical dermatology, both for teaching and clinical research.
In conclusion, this clinical case highlights an atypical manifestation of molluscum pendulum in the plantar region, an infrequent location for this type of benign lesion. The prolonged evolution of the lesion without significant symptoms underscores the importance of differential diagnosis, especially in weight-bearing areas where biomechanical characteristics can influence clinical presentation and therapeutic options. Surgical excision with advancement flap closure proved to be an effective strategy for complete removal of the lesion, minimizing the risk of recurrence and optimizing healing. This approach highlights the relevance of adapting surgical techniques based on the patient’s individual location and characteristics.
Authors‘ contributions
Conception and design of the study: JMCM.
Data collection: RRR, SSM.
Creation, writing, and drafting: RRM, AMRP.
Final review: JMCM, RGP.
Conflicts of interest
None declared.
Funding
None declared.
References
- Ben Hassouna W, Ben Bachouche W, Bouzaiene H, Chargui R, Khomsi F, Habib Mtaalah M, et al. Molluscum pendulum géant du sein. Ann Dermatol Venereol. 2007;134:72-8. DOI: 10.1016/S0151-9638(07)88997-6.
- Choudhary ST. Treatment of unusually large acrochordon by shave ecision and electrodesiccation. J Cutan Aesthet Surg. 2008;1(1):21-2. DOI: 10.4103/0974-2077.41153.
- Weedon D. 34 - Tumors and tumor-like proliferations of fibrous and related tissues. En: Weedon D (editor). Weedon’s Skin Pathology. 3.ª ed. Churchill Livingstone; 2010. p. 809-844.e29. DOI: 10.1016/B978-0-7020-3485-5.00035-8.
- Banik R, Lubach D. Skin tags: Localization and frequencies according to sex and age. Dermatologica. 1987;174(4):180-3. DOI: 10.1159/000249169.
- Akpinar F, Dervis E. Association between acrochordons and the components of metabolic syndrome. Eur J Dermatol. 2012;22(1):106-10. DOI: 10.1684/ejd.2011.1572.
- Rasi A, Soltani-Arabshahi R, Shahbazi N. Skin tag as a cutaneous marker for impaired carbohydrate metabolism: A case-control study. Int J Dermatol. 2007;46(11):1155-9. DOI: 10.1111/j.1365-4632.2007.03287.x.
- Dharmapuri G, Francis GB, Sivaraman AP. Giant acrochordon of labia majora: An uncommon manifestation of a common disease. J. Evolution Med. Dent. Sci. 2016;5(87):6521-2.
- Al-Dhalimi MA, Al-Janabi MH. Carbon dioxide laser treatment of skin tags. J Dermatol Treat. 2007;18(2):94-6.
- Al-Mutairi N. Associated cutaneous diseases in obese adult patients: A prospective study from a skin referral care center. Med Princ Pract. 2011;20(3):248-52. DOI: 10.1159/000323597.
- Barraya L, Nakpane E. Abdomen molluscum; pendulous abdomen; repair; new umbilicus. Presse Med (1893). 1968;76(48):2287-9.
- Chachava MK, Gotsiridze TI. Plastic surgery in pendulous abdomen. Vestn Khir Im I I Grek. 1972;107(1):89-93.
- Köseo?lu HG, Bozca BC, Ba?sorgun C?, Sar? R, Akba? SH, Karaka? AA. The role of insulin-like growth factor in acrochordon etiopathology. BMC Dermatol. 2020;20(1):14. DOI: 10.1186/s12895-020-00111-0.
- Hirt PA, Castillo DE, Yosipovitch G, Keri JE. Skin changes in the obese patient. J Am Acad Dermatol. 2019;81(5):1037-57. DOI: 10.1016/j.jaad.2018.12.070.
- Saritas S, Tekin HG, Høgsberg T, Hölmich LR, Juel J. Benign skin tumours. Ugeskr Laeger. 2022;184(29):V10210786.
- Higgins JC, Maher MH, Douglas MS. Diagnosing common benign skin tumors. Am Fam Physician. 2015;92(7):601-7.
- Graells J, Espinola A, Barrio C, Muñoz MD, Román A, Parellada N. Cirugía menor ambulatoria dermatológica y crioterapia. Estudio comparativo entre un dermatólogo y médicos de familia. Actas Dermosifiliogr. 2007;98(3):171-7. DOI: 10.1016/S0001-7310(07)70041-8.
- Bahce ZS, Akbulut S, Sogutcu N, Oztas T. Giant acrochordon arising from the thigh. J Coll Physicians Surg Pak. 2015;25(11):839-40.
- Luba MC, Bangs SA, Mohler AM, Stulberg DL. Common benign skin tumors. Am Fam Physician. 2003;67(4):729-38.
- Triwatcharikorn J, Itthipanichpong Y, Washrawirul C, Chuenboonngarm N, Chongpison Y, Udomsawaengsup S, et al. Skin manifestations and biophysical changes following weight reduction induced by bariatric surgery: A 2-year prospective study. J Dermatol. 2023;50(12):1635-9. DOI: 10.1111/1346-8138.16951.