DOI: http://dx.doi.org/10.20986/revesppod.2023.1673/2023
ORIGINAL
Rotational anomalies in women with hallux valgus. Observational study
Anomalías rotacionales en mujeres con hallux valgus. Estudio observacional
Rosana Giménez López1
1Escuela de Doctorado. Universidad Católica de Valencia “San Vicente Mártir”. Valencia, España
Abstract
Objectives: To analyze differences in laterality in rotational and torsional movement in the lower extremity and its possible influence on the development of hallux abductus valgus.
Patients and methods: The sample included 129 women. The degree of severity of hallux abductus valgus, hip rotation, tibial torsion, mobility of the first metatarsophalangeal joint, foot posture index, and foot progression angle were evaluated.
Results: Our results showed that there were differences in external rotation between both hips of 2.34° (p < 0.001) and between internal and external rotation of the left hip of 4.11° (p < 0.002). We also found a difference of the foot progression angle between feet of 3° (p < 0.001), but there was no significant difference between tibial torsion and foot posture index (p > 0.05). A difference in range of motion was found between both first metatarsophalangeal joints of 6.30° (p < 0.001), and a relationship was found between extension and range of motion of the first metatarsophalangeal joint and hallux abductus valgus (p < 0.05).
Conclusions: Based on the results obtained in this sample, the data points to a greater range of motion of the first metatarsophalangeal joint in the left foot. The results also indicate a probable predominance of internal rotation of the left extremity and external rotation of the right extremity, which did not show asociation with the degree of hallux aductus valgus in this study.
Keywords: First metatarsophalangeal joint, hallux valgus, lower extremity, torsion, rotation.
Resumen
Objetivos: Analizar las diferencias de lateralidad en el movimiento de rotación y torsión en la extremidad inferior y su posible influencia en el desarrollo del hallux abductus valgus.
Pacientes y métodos: La muestra incluyó 129 mujeres. Se evaluó el grado de severidad del hallux abductus valgus, la rotación de cadera, la torsión tibial, la movilidad de la primera articulación metatarsofalángica, el índice postural del pie y el ángulo de progresión del pie.
Resultados: Nuestros resultados mostraron que existían diferencias en la rotación externa entre ambas caderas de 2.34° (p < 0.001) y entre la rotación interna y externa de la cadera izquierda de 4.11° (p < 0.002). También se encontró una diferencia del ángulo de progresión del pie de 3° (p < 0.001), pero no hubo diferencias significativas entre la torsión tibial y el índice postural del pie (p > 0.05). Se encontró una diferencia en el rango de movimiento entre ambas primeras articulaciones metatarsofalángicas de 6.30° (p < 0.001), y se halló una relación entre la extensión y el rango de movimiento de la primera articulación metatarsofalángica y el hallux abductus valgus (p < 0.05).
Conclusiones: En base a los resultados obtenidos en esta muestra, los datos apuntan a un mayor rango de movimiento de la primera articulación metatarsofalángica en el pie izquierdo. Los resultados también indican un probable predominio de rotación interna de la extremidad izquierda y de rotación externa de la extremidad derecha, que no mostraron asociación con el estadio del hallux abductus valgus en este estudio.
Palabras clave: Primera articulación metatarsofalángica, hallux valgus, extremidades inferiores, torsión, rotación.
Recibido: 30-07-2023
Aceptado: 23-11-2023
Correspondence: Rosana Giménez López
rosana.gimenez@mail.ucv.es
Introduction
Hallux abductus valgus (HV) is the most common progressive three-dimensional deformity of the forefoot. It consists of a misalignment and medialization of the first metatarsal with the formation of a medial bony prominence, as well as lateralization of the first toe, with or without pronation. The development of the deformity involves the imbalance of the soft tissues of the midfoot and forefoot. Its causes are intrinsic and extrinsic, and the deformity can cause pain and decreased mobility, among other alterations(1,2,3,4).
Rotational and torsional asymmetries of the lower limbs have been constantly observed in scientific literature. These asymmetries can generate compensatory deviations during gait and promote pathologies in the lower extremities (LE), such as osteoarthritis(5,6). Femoral anteversion and tibial torsion (TT) are the most frequently reported asymmetries. External TT in the right lower extremity (RLE) is described in the literature with an increase between 1 and 5° with regard to the left lower extremity (LLE) (7,8,9). The increase of internal femoral anteversion in LLE is also widely described by various authors (8,9,10,11,12), whose value is found to be increased between 1 and 7° in regard to RLE. Recently, Ries et al. (13) reported a left femoral anteversion of 2.2° higher than the right, a right external TT that increased by 2.8°, and a total of 5.1° more external rotation in RLE, with an absolute rotation difference of 9.5° between both limbs. The influence of TT on the angle of foot progression has also been observed (12,14).
Several studies such as those by Jeon et al.(15), Sass and Hassan (16), and Requeiro et al. (17) have reported that the rotational asymmetry found during childhood and later in adulthood has its origin in embryonic development from the adoption of a specific fetal position during gestation, hereditary factors, or the adoption of flawed positions after birth; however this last factor may be due to the position adopted during gestation and not be a predisposing factor in itself, according to Rodriguez et al. (18). Staheli (19) specifically points out that internal torsion and metatarsus aductus would be conditioned by the intrauterine fetal position. The lower extremities begin to rotate internally from the seventh week of gestation to adapt to the uterine space. At present, the mechanism that manages the position of the lower limbs to adapt to each other in the uterine space and acquire a specific position throughout the gestational period seems to be unclear. Studies in vertebrates point to the role of the Hox genes, which direct the anteroposterior plane according to spatial and temporal collinearity principles and are also found in mammals (20,21). This adaptive process of the LE can condition torsional and rotational asymmetry of the limbs after birth, leading to an inability of rotational and torsional normalization of the LE during the development of the individual, ultimately favoring a certain asymmetry in adulthood. At the podiatric level, more studies identifying the differences in gender and laterality have been observed, but they are still scarce. Although previous work has studied the influence of torsions and rotations in the foot, how these laterality rotational differences may influence the onset and development of HV has not yet been studied.
The present study performed a comparison of HV severity stages and analyzed the range of rotation of the hip joint, TT, first metatarsophalangeal joint (1st MTPJ), foot posture index (FPI), and foot progression angle (FPA) individually and together in patients with HV. The aim was to identify laterality differences in the lower limbs and their possible relationship with the degree of HV severity.
Patients and methods
Participants
For this study, a previous non-probabilistic and consecutive sampling was performed in a podiatry clinic from January 2021 to February 2022. The subjects were patients that attended for various reasons and presented with HV, regardless of their stage. First, a triage by gender was not performed to determine the prevalence of men and women with HV. Of the total of 144 participants, 129 were women (89.58 %) and 15 (10.42 %) were men. Given the resulting disparity between the two sexes, the sample of participants with the highest number of cases of HV was analyzed to avoid possible bias in the variables of the joint range of motion. The sample consisted of a total of 129 women with a mean age of 51 ± 11 years and a BMI of 25.10 ± 4.68. The subjects’ predisposition to use the right or left limbs was not considered in this study, although approximately 95% were right-footed, which was determined by asking with which foot they would kick a ball.
Inclusion criteria for the study were women aged between 20 and 70 years and had HV, regardless of the level of the deformity. Written informed consent was obtained from all participants prior to clinical examination.
Exclusion criteria were patients with a history of musculoskeletal pathology, surgery, or previous orthopedic treatment. Patients with hallux limitus (extension less than 65°) (22) and patients with infra- or supraduction of the first or second toe were excluded from the study.
Study Protocol
A cross-sectional, observational, analytical study was conducted. The sample calculation was performed to estimate the proportion of patients with HV who present rotational differences in the LE. A sample size of 93 patients were needed to estimate this proportion for a confidence level of 95 % and a precision of ± 10 percentage units, with a prediction that this proportion would be around 60 %.
Passive internal and external hip rotation was measured in the prone position with a 90° genuflexion by means of an analog inclinometer placed on the tibial margin (23). The patient was instructed not to elevate the opposite hip during hip rotation or during the leg relaxation movement to both sides. Tibial torsion was assessed by means of a two-branch universal goniometer; one of the branches was positioned on the sole of the foot, tracing the bisector from the center of the heel to the second radius, and the other branch was directed to the sagittal center of the thigh, maintaining the position of the neutral subtalar joint24. In the 1st MTPJ, passive flexion and extension were assessed by placing the goniometer on the internal of the foot, with a branch of the goniometer following the previously-traced bisector of the first radius and the proximal phalanx, after which the corresponding movement was forced to its articular stop (25) (Figure 1).
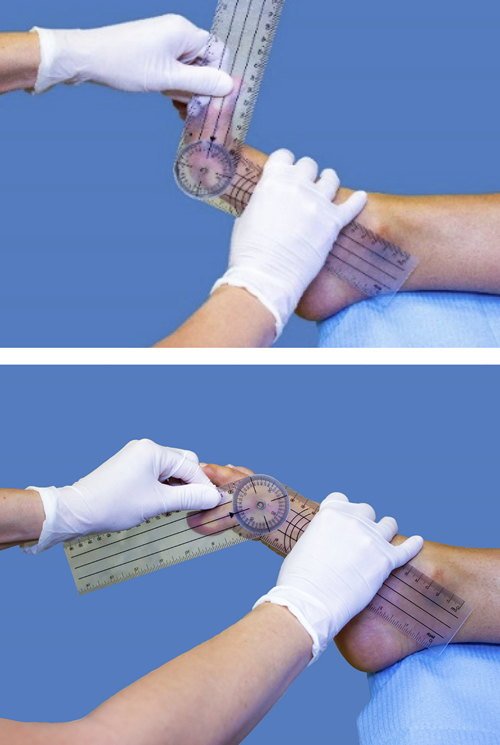
Figure 1. First metatarsophalangeal joint measurement with a goniometer.
To obtain the average value, measurements were taken on three consecutive occasions, alternating both feet. All measurements were taken by a single examiner with 20 years of clinical experience as a podiatrist. The stage of HV was assessed using photographs and the Manchester Visual Scale (26). This scale consists of standardized photographs of feet with four degrees of HV (none [A], mild [B], moderate [C], and severe [D]). The FPA was assessed using the T-Plate® pressure platform (Medicapteurs, France) with 1,600 resistive sensors of 10 × 10 mm, with an active surface of 400 × 400 mm27, recording an average of five steps for each foot at the individual and natural cadence of each patient. Subsequently, the angle measurement program, Ruler® (designed by Ergonautas, Polytechnic University of Valencia), was used to measure the angle of progression of each foot. The FPI-6 was evaluated, and was composed of six items to classify the position of the feet: palpation of the talar head, observation of supramalleolar/inframalleolar curvature, inversion/eversion of the calcaneus, medial prominence of the talonavicular joint, heigh of the medial arch, and abduction/adduction of the toes viewed from the rearfoot. The score range is from -12 to +12. The reference standards are: normal, 0 to +5; pronated, +6 to +9; highly pronated, +10 to +12; supinated, -1 to -4; highly supinated, -5 to -1228.
Statistical analysis
The study was performed using R statistical software, version 4.2.0. First, a descriptive analysis of the quantitative variables was performed using minimum, maximum, mean, median, and standard deviation, and the categorical variables were studied using absolute and relative frequencies. The assessment of hip rotation laterality, TT, mobility of the 1st MTPJ, FPI, and FPA was performed using the paired samples t-test or Wilcoxon rank sum test in case of non-compliance with normality. To observe possible statistically significant relationships in each pair of quantitative variables, hip rotation, TT, and mobility of the 1st MTPJ, FPI, FPA, and linear regression models were studied using Pearson’s correlation coefficient. To study the relationship between Manchester grades (B, C, D), hip rotation, TT, mobility of the 1st MTPJ, and FPA, multinomial logistic regression models were fitted.
Results
The asymmetry between internal and external rotation in LLE was statistically significant. The estimated value for the mean difference between both internal rotation was 4.11° (95 % confidence interval: 1.47-6.74). The descriptive data indicates that the internal movement in the left hip was greater (p = 0.002). Significant differences were found between the right and left side for the external rotation variable, with a mean estimate difference of 2.34 units (95 % confidence interval: 1.07-3.61, p < 0.001). There was also a difference in hip range of motion (ROM), with a mean difference of 2.12 units (95 % confidence interval: 0.54-3.70, p < 0.008) (Figure 2). Regarding tibial torsion, no statistically-significant difference was found in TT between both LE at 0.75° (95 % confidence interval: -0.002-1.50, p = 0.05).
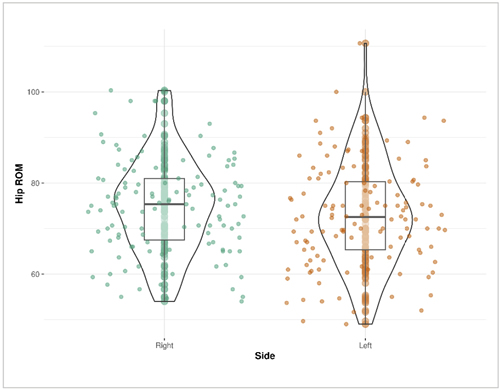
Figure 2. Hip range of motion (ROM) difference by side.
The results show no evidence that the variable FPI differs in the right 2.44 ± 3.41 and left 2.51 ± 3.44 sides. The estimated mean value was -0.024 (-0.408 and 0.359), with p > 0.05. Table 1 describes the summary statistics of the variables.
Table I. Statistics summary of the variables measured in the study.
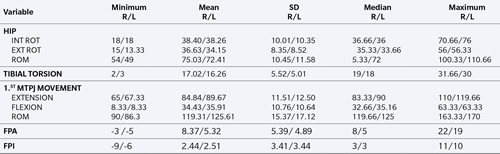
R: right. L: left. INT ROT: internal rotation. EXT ROT: external rotation. ROM: range of motion. 1ST MTPJ: first metatarsophalangeal joint. FPA: Foot pregression angle. FPI: Foot posture index.
The difference between the right and left foot progression angle was 3° (95 % confidence interval: 2.20-3.90, p < 0.001) (Figure 3).
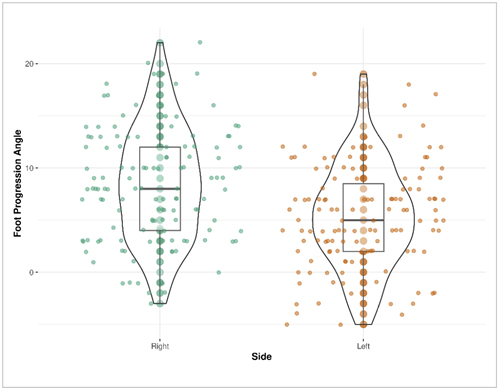
Figure 3. Foot progression angle difference by side.
Regarding the mobility of the 1st MTPJ, the difference found in flexion was 1.50° (95 % confidence interval: 0.33-3.33, p < 0.016), in extension was 4.66° (95 % confidence interval: 3, 16-6.15, p < 0.001), and ROM was 6.30° (95 % confidence interval: 4.44-8.15, p < 0.001), and furthermore, all values were higher in the left MTPJ (Table 2). The presence of HV in the sample of 129 subjects was observed bilaterally in 123 cases (95.34 %) and unilaterally in 6 cases (4.65 %): one (0.77 %) in the right foot and five (3.87 %) in the left foot. In the level of severity of HV, stage B increased in eight cases (8.06 %) in the right feet, according to Manchester scale(26). Furthermore, the left feet presented an increase of seven (4.85 %) more cases of HV in stage C, and five (3.82 %) more cases in stage D, but no statistically-significant differences were observed between both feet (Odds Ratio (OR)B: 0.86, p = 0.420; OR C: 1.33, p = 0.266; and OR D: 2.11, p = 0.163). For both left and right foot Manchester stage, no significant effect of hip rotation, TT (Figure 4), FPI (Figure 5) or FPA (Figure 6) was found (p > 0.05). Table 2 describes the values of the variables according to the degree of severity of HV (Table 2).
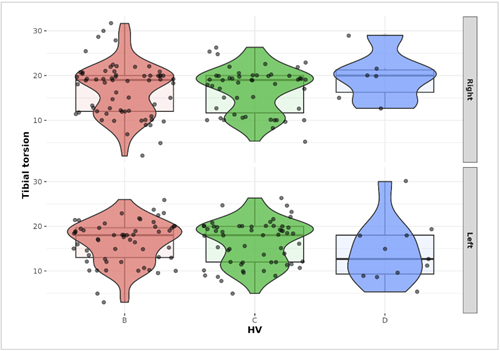
Figure 4. Relationship between Hallux valgus (HV) and tibial torsion (TT).
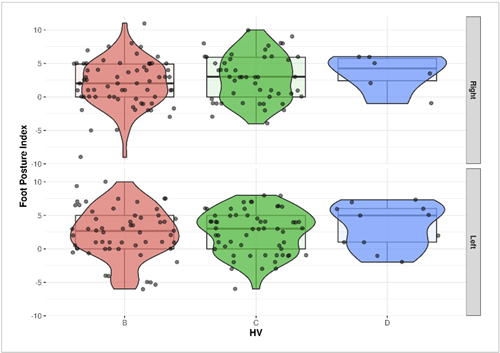
Figure 5. Relationship between Hallux valgus (HV) and Foot posture index (FPI).
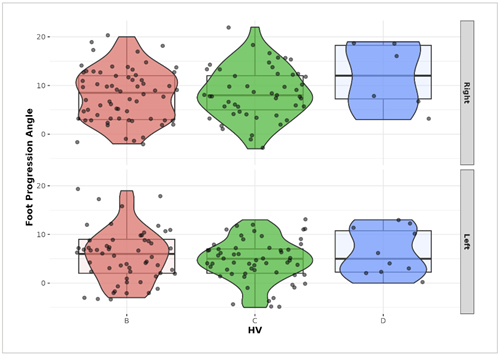
Figure 6. Relationship between Hallux valgus (HV) and Foot progression angle (FPA).
Regarding the mobility of the 1st MTPJ, a significant effect was found for the Manchester degree in extension in both feet and range of motion in the left foot (Table 2). Each one-degree increase of extension reduces the probability of having a type C HV in regard to B by 3.6 % in the right foot. In the left foot, it reduces the probability of having a type D HV in regard to B by 5.8 %. Each one-degree increase in ROM reduces the probability of having a type D HV in regard to B by 4.6 % in the left foot.
Table II. Average values according to hallux abductus valgus.
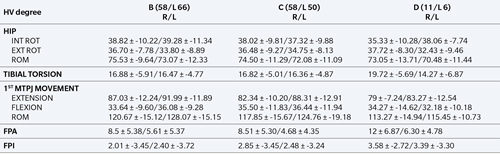
R: right. L: left. INT ROT: internal rotation. EXT ROT: external rotation. ROM: range of motion. 1ST MTPJ: first metatarsophalangeal joint. FPA: foot pregression angle. FPI: foot posture index.
Discussion
Until now, rotational and torsional asymmetries in the LE and their possible impact on the development of HV had not been analyzed. The results of this study reveal the possible existence of a left internal rotational pattern in LLE and a right external rotational pattern in RLE, as observed in previous studies such as Ries (13) and Lafuente et al. (29).
In terms of percentages of involvement, the study by Mathon(9), using two different methods of measurement, revealed a difference in TT of 3° in 12 % of the sample with the first method, and 4.9° in 9 % of the participants with a second method. Shultz and Nguyen(30) also reported a difference in TT that exceeded the measurement error in more than 32 % of the participants. Regarding femoral anteversion, Mathon et al.(9) found an absolute side difference of 6.3° in 47 % of participants, and Shultz et al. (31) found a difference between 5 % and 32 % of cases. The analysis of the data in this study reveals that neither hip rotational asymmetry nor TT is related to the stage of severity of HV in any foot, although there is a tendency for values to decrease in the left leg and increase in the right leg as the stage of severity of the HV increases. Despite this, this LE asymmetry may influence the foot during gait as the result of the FPA shown.
In this study, measurements in the LE were taken segmentally rather than globally to identify the origin of a rotational abnormality in the lower limb as a whole. Singh(32) and Hawi(24) argue that the thigh-foot angle provides a reliable alternative to computed tomography for measuring TT. The results of this study do not deviate from the average 15° thigh-foot angle in people without pathology (33), although this value can be extended to 19°(34). In scientific literature, a difference of less than 3° is not considered clinically significant(35), although, it is observed that even with lower values, TT is increased in RLE compared to LLE.
With regard to other studies, the hip rotation values do not differ from the mean values referenced in healthy subjects(36), demonstrating a predominance of internal rotation versus external rotation, in contrast with the American Academy of Orthopedic Surgeons referenced data(37). In this regard, other authors such as Shultz and Nguyen(30) reported that women had greater internal rotation of the hips and genu valgum compared to men. Along the same lines, the studies by Hudson14 and Cannon et al. (38) reported a predominance of internal hip rotation versus external rotation associated with internal femoral torsion in a higher percentage of women. In this study, it is noted that increased external rotation in the right hip is associated with external TT in twice as many cases as with internal TT, and on the contrary, in the left hip, internal rotation is normally associated with internal TT.
An internal rotational and torsional component in the LE will favor a greater pronation of the foot. In addition, this circumstance favors the medial ligaments at the level of the 1st MTFJ for elongation, and the head of the first metatarsal for sliding medially, accentuating the imbalance of the joint reaction forces(39). This may be the reason why we found a higher passive ROM of the left 1st MTFJ, which may be related to the more severe cases of HV found in the left foot at 9 %. These data do not coincide with the recent study by Crooks et al.(40), which evaluated the difference between sides in cases of HV, showing only 2 % more severe cases in the left foot. The present study, in contrast to Crooks, included unilateral cases in the sample and used a different methodology. Likewise, the mobility values of this joint without weight bearing are observed to be increased with respect to other studies performed with the same methodology(41). One of the causes of this increase in joint mobility could be the composition of the sample, which was represented only by women whose ligamentous laxity is usually found in a higher proportion (3:1) with respect to men (42). The mean FPI value observed by Sanchez et al. (28) was 1.6 in men and 2.4 in women, similar to the results of this study, and these were related to more supinated feet in men and more valgus or neutral feet in women. In turn, Carvalho et al.(43) observed that the participants in their study had a more pronated posture of the left foot than the right.
In this study however, the FPI result corresponds to normal feet and does not evidence the pronator character in the left foot, supposedly favored by the internal rotation observed in LLE. We found that the frontal plane position values of the calcaneus of the FPI were higher in the left foot, and lower in the right foot, with respect to the average. In addition, according to Livingston´s article(44), mean values did not always reflect the real variation of the data within the sample. It was found that in 56 % of the participants there was a minimum difference of 4° in the bilateral hindfoot angle that exceeded 7° in 20 % of the sample; however, Nguyen and Shultz(45) did not observe differences between sides or sexes in this criterion.
Moreover, when excluding feet with hallux limitus in this study, a greater number of right feet with hallux limitus was observed at 5:2 with respect to the left. Although this is a low number, we hypothesize the influence of increased external TT and external hip rotation as a predisposing factors for foot supination. This supination would lead to elevation of the first metatarsal off the ground, or in other words, to a metatarsus primus elevatus, thus favoring a hallux limitus. This new hypothesis would be supported by the research of Ciufo (46), who observed a statistically-significant correlation between external TT, talus morphology, and tibiotalar inclination. With reference to this alteration and with another view, Lafuente et al. (47) identified hallux limitus as the cause of a lower internal rotation of the EI; however, the cause-effect of this other deformity is not clear. We also found other references to asymmetry, such as that of foot height by Zhao (48), who observed more height at the right foot with respect to the left, which could be explained by a mostly-supinated position of the right foot, or a pronated position of the left foot. Throughout the growth of the individual, the foot progression angle remains slightly positive, with values between 6° to 10°, due to the progressive loss of hip internal rotation(7). The average FPA in this study was slightly decreased in the left foot. This decrease may be due to greater femoral anteversion, as indicated by Alexander (5) and Bruderer et al.6, although according to Hudson’s assessment (14), TT would be the component that would most influence the direction and magnitude of the FPA, as shown by 68 % of the subjects in his study.
Regarding the results of this analysis, a 3° difference was found in the angle of progression between both feet coinciding with the sum of the rotational asymmetries of the RLE in unloading, which is very similar to those of other studies carried out with children (49,50), so it can be assumed that this asymmetry persists into adulthood.
In most of the articles consulted, it was found that the participants did not present pathology, which indicates that these asymmetries may have an influence on the appearance and development of HV, depending on other predisposing morphological factors in the individual. This study suggests that the biomechanics of the human body are not always able to achieve rotational symmetry of the limbs during its development. Data from this study indicates a predominance of left internal and right external rotation in adulthood due to fetal position and/or hereditary factors. Hereditary factors are still a pending study, and the fetal position that would lead to this asymmetry would have its origin in the placement of the right lower extremity over the left during gestation, favoring greater internal rotation of the LLE and greater external rotation of the RLE, as pointed out by several authors such as Sthaeli (19), Fabry (10), Radler(12), Sass and Hassan(16), and Rodriguez (18) (Figure 7). Along these lines, Katz51 observed that premature infants presented a greater external rotational pattern in their lower extremities, and a lesser number of adducted metatarsals. Furdon and Donlon(52) emphasize that the foot is malleable, so it is susceptible to compression and deformation due to the intrauterine position. The authors also point out the importance of distinguishing between a temporary positional deformity and a structural malformation of the foot, which is a challenge. This statement could also be extrapolated to the lower limb as a whole.
Figure 7. Drawing “the fetus in the womb” by Leonardo Da Vinci. Source: Wikipedia.
In the absence of better performance and accessibility of diagnostic imaging systems, such as computed tomography, great similarities between these sophisticated techniques can be found with those used in a podiatry clinic through rudimentary tools; for example, a universal goniometer, which facilitates the possible reproducibility of this study in any field. This study has limitations due to the exclusion criteria, which has led to a possible decrease in the information recorded on variables such as the severity of HV. Also, it was not possible to access a control sample due to the COVID-19 pandemic situation during data collection. Nevertheless, we found the same rotational asymmetries in the LE as in samples without pathology according to the literature consulted. It is important to emphasize that the mobility of the joints is assessed in unloading, so these data should be contrasted with the global performance and dynamics of the LE.
In conclusion, the findings of the present study have shown no significant difference between right and left HV, though there was a significant difference in ROM of the 1st MTFJ, being greater in the left foot. There was a difference between both hips rotations but no difference was observed in TT. Our study points to the possible existence of a frequent internal rotation pattern in the LLE and external in the RLE to be considered in the early diagnosis and treatment of the individual. Fetal position could be the common predisposing factor of a rotational pattern of LE in a high percentage of the population. Whose origin could be dueto a “Lower limbs gestational positional pattern”. These rotational asymmetries of the LE may condition the structure and function of the of the musculoskeletal system, of the foot and the 1st MTFJ. Future biomechanical and other investigations will be pertinent to corroborate these results.
Acknowledgements
To my tutor, Mr. Carlos Barrios Pitarque, for his help at every stage of this study. To Carlos Peña and Juan Antonio Carbonell from INCLIVA for their constant advice, and to the Scientific Committee of the Revista Española de Podología for evaluating this study for publication as a scientific article.
Ethics Declaration
This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Research Ethics Committee of the Unviersidad Católica de Valencia San Vicente Mártir (CEI) on 21 Januarty 2021. Project code: UCV/2020-2021/052.
Conflict of interest
The author declares that she has no economic or commercial interest.
Funding
None.
References
- Zirngibl B, Grifka J, Baier C, Götz J. Hallux valgus: Ätiologie, diagnostische und therapeutische Prinzipien. Orthopade. 2017;46(3):283-96. DOI: 10.1007/s00132-017-3397-3.
- Shi GG, Whalen JL, Turner NS 3rd, Kitaoka HB. Operative approach to adult hallux valgus deformity: Principles and techniques. J Am Acad Orthop Surg. 2020;28(10):410-18. DOI: 10.5435/JAAOS-D-19-00324.
- de Cesar Netto C, Richter M. Use of advanced weightbearing imaging in evaluation of hallux valgus. Foot Ankle Clin. 2020;25(1):31-45. DOI: 10.1016/j.fcl.2019.10.001.
- Ray JJ, Friedmann AJ, Hanselman AE, Vaida J, Dayton PD, Hatch DJ, et al. Hallux valgus. Foot Ankle Orthop. 2019;4(2):2473011419838500. DOI: 10.1177/2473011419838500.
- Alexander N, Wegener R, Lengnick H, Payne E, Klima H, Cip J, et al. Compensatory gait deviations in patients with increased outward tibial torsion pre and post tibial derotation osteotomy. Gait Posture. 2020;77:43-51. DOI: 10.1016/j.gaitpost.2020.01.011.
- Bruderer-Hofstetter M, Fenner V, Payne E, Zdenek K, Klima H, Wegener R. Gait deviations and compensations in pediatric patients with increased femoral torsion. J Orthop Res. 2015;33(2):155-62. DOI: 10.1002/jor.22746.
- Gruskay JA, Fragomen AT, Rozbruch SR. Idiopathic rotational abnormalities of the lower extremities in children and adults. JBJS Rev. 2019;7(1):e3. DOI: 10.2106/JBJS.RVW.18.00016.
- Eckhoff DG, Jacofsky DJ, Springer BD, Dunbar M, Cherian JJ, Elmallah RK, et al. Bilateral symmetrical comparison of femoral and tibial anatomic features. J Arthroplasty. 2016;31(5):1083-90. DOI: 10.1016/j.arth.2015.11.021.
- Mathon P, Micicoi G, Seil R, Kacaoglu B, Cerciello S, Ahmad F, et al. Healthy middle-aged Asian and Caucasian populations present with large intra- and inter-individual variations of lower limb torsion. Knee Surg Sports Traumatol Arthrosc. 2021;29(4):1083-89. DOI: 10.1007/s00167-020-06096-0.
- Fabry G, Cheng LX, Molenaers G. Normal and abnormal torsional development in children. Clin Orthop Relat Res. 1994;(302):22-6. DOI: 10.1097/00003086-199405000-00005.
- Bleck EE. Developmental orthopaedics. III: Toddlers. Dev Med Child Neurol. 1982;24(4):533-55.
- Radler C, Kranzl A, Manner HM, Höglinger M, Ganger R, Grill F. Torsional profile versus gait analysis: consistency between the anatomic torsion and the resulting gait pattern in patients with rotational malalignment of the lower extremity. Gait Posture. 2010;32(3):405-10. DOI: 10.1016/j.gaitpost.2010.06.019.
- Ries C, Boese CK, Ott N, Doerner J, Müller LP, Hackl M. Intra-individual variance of bilateral femoro-tibial leg rotation: a CT study of 105 healthy subjects. Knee Surg Sports Traumatol Arthrosc. 2021;29(4):1106-13. DOI: 10.1007/s00167-020-06101-6.
- Hudson D. A comparison of ultrasound to goniometric and inclinometer measurements of torsion in the tibia and femur. Gait Posture. 2008;28(4):708-10. DOI: 10.1016/j.gaitpost.2008.04.017.
- Jeon JH, Yoon YS, Lee KJ, Yu KP, Lee JH, Seog TY, et al. A new instrument for measuring tibial torsion in pediatric patients. Ann Rehabil Med. 2017;41(3):441-49. DOI: 10.5535/arm.2017.41.3.441.
- Sass P, Hassan G. Lower extremity abnormalities in children. Am Fam Physician. 2003;68(3):461-68.
- Requeiro Molina JJ, Izaquirre Martínez Y, Machado Consuegra A, Requeiro Molina GM, Morejón Fernández JM, Rodríguez Medina O. Influencia de las posturas al sentarse y dormir en la aparición de deformidades del sistema musculoesquelético en el niño. MediSur. 2005;3(3):37-54.
- Rodríguez, JC. Adoptar una posición que parece inadecuada: ¿es vicio postural o hace parte del desarrollo normal de la postura? Revista Ciencias de la Salud. 2003;1(1):58-67.
- Staheli LT. In-toeing and out-toeing in children. J Fam Pract. 1983;16(5):1005-11.
- Antonelli M, Rosas C, Rojas M. Limb development in vertebrates. Int J Morphol. 2012;30:1512-19. DOI: 10.4067/S0717-95022012000400040.
- Hrycaj SM, Wellik DM. Hox genes and evolution. F1000Res. 2016;5:F1000 Faculty Rev-859. DOI: 10.12688/f1000research.7663.1.
- Hernández V. Análisis de las variables baropodométricas en el tratamiento ortopodológico del Hallux Limitus. 2021. Tesis de doctorado. UCAM.
- Souza TR, Mancini MC, Araújo VL, et al. Clinical measures of hip and foot-ankle mechanics as predictors of rearfoot motion and posture. Man Ther. 2014;19(5):379-85. DOI: 10.1016/j.math.2013.10.003.
- Hawi H, Kaireit TF, Krettek C, Liodakis E. Clinical assessment of tibial torsion differences. Do we always need a computed tomography?. Eur J Trauma Emerg Surg. 2022;48(4):3229-35. DOI: 10.1007/s00068-022-01884-4.
- Zammit GV, Munteanu SE, Menz HB. Development of a diagnostic rule for identifying radiographic osteoarthritis in people with first metatarsophalangeal joint pain. Osteoarthritis Cartilage. 2011;19(8):939-45. DOI: 10.1016/j.joca.2011.04.010.
- Menz HB, Munteanu SE. Radiographic validation of the Manchester scale for the classification of hallux valgus deformity. Rheumatology (Oxford). 2005;44(8):1061-66. DOI: 10.1093/rheumatology/keh687.
- Cobos-Moreno P, Astasio-Picado Á, Martínez-Nova A, Sánchez-Rodríguez R, Escamilla-Martínez E, Gómez-Martín B. The Podoprint® plantar pressure platform: Evaluation of reliability and repeatability, and determination of the normality parameters. J Tissue Viability. 2022;31(4):619-24. DOI: 10.1016/j.jtv.2022.07.005.
- Sánchez Rodríguez R, Martínez Nova A, Escamilla Martínez E, Gómez Martín B, Martínez Quintana R, Pedrera Zamorano JD. The foot posture index: anthropometric determinants and influence of sex. J Am Podiatr Med Assoc. 2013;103(5):400-04. DOI: 10.7547/1030400.
- Lafuente Sotillos G, Lafuente Fuster B, López Carrero E, Talamino Delgado E. Reflexiones sobre la torsión tibial externa y repercusiones en la biomecánica. Rev Esp Pod 2022;33(2):128-33. DOI: 10.20986/revesppod.2022.1652/2022.
- Shultz SJ, Nguyen AD, Schmitz RJ. Differences in lower extremity anatomical and postural characteristics in males and females between maturation groups. J Orthop Sports Phys Ther. 2008;38(3):137-49. DOI: 10.2519/jospt.2008.2645.
- Shultz SJ, Nguyen AD. Bilateral asymmetries in clinical measures of lower-extremity anatomic characteristics. Clin J Sport Med. 2007;17(5):357-61. DOI: 10.1097/JSM.0b013e31811df950.
- Singh H, Gupta P, Kaur R, Sharma C. Comparison of clinical with CT based evaluation for tibial torsion. J Clin Orthop Trauma. 2022;29:101875. DOI: 10.1016/j.jcot.2022.101875.
- Davids JR, Davis RB. Tibial torsion: significance and measurement. Gait Posture. 2007;26(2):169-71. DOI: 10.1016/j.gaitpost.2007.05.002.
- Nguyen AD, Shultz SJ. Sex differences in clinical measures of lower extremity alignment. J Orthop Sports Phys Ther. 2007;37(7):389-98. DOI: 10.2519/jospt.2007.2487.
- Hallaçeli H, Uruç V, Uysal HH, et al. Normal hip, knee, and ankle range of motion in the Turkish population. Acta Orthop Traumatol Turc. 2014;48(1):37-42. DOI: 10.3944/AOTT.2014.3113.
- Kouyoumdjian P, Coulomb R, Sanchez T, Asencio G. Clinical evaluation of hip joint rotation range of motion in adults. Orthop Traumatol Surg Res. 2012;98(1):17-23. DOI: 10.1016/j.otsr.2011.08.015.
- American Academy of Orthopedic Surgeons: Joint Motion: Method of measuring and recording, Chicago, IL: American Academy of Orthopedic Surgeons; 1965.
- Cannon A, Finn K, Yan Z. Comparison of hip internal and external rotation between intercollegiate distance runners and non-running college students. Int J Sports Phys Ther. 2018;13(6):956-62. DOI: 10.26603/ijspt20180956.
- Steadman J, Barg A, Saltzman CL. First metatarsal rotation in hallux valgus deformity. Foot Ankle Int. 2021;42(4):510-22. DOI: 10.1177/1071100721997149.
- Crooks SA, Lewis TL, Ray R, Gordon DJ. Symmetry of bilateral hallux valgus deformity: A radiographic study. Clin Anat. 2022;35(4):414-20. DOI: 10.1002/ca.23772.
- Frimenko RE, Lievers W, Coughlin MJ, Anderson RB, Crandall JR, Kent RW. Etiology and biomechanics of first metatarsophalangeal joint sprains (turf toe) in athletes. Crit Rev Biomed Eng. 2012;40(1):43-61. DOI: 10.1615/CritRevBiomedEng.v40.i1.30.
- Carbonell-Bobadilla N, Rodríguez-Álvarez AA, Rojas-García G, Barragán-Garfias JA, Orrantia-Vertiz M, Rodríguez-Romo R. Síndrome de hipermovilidad articular. Acta ortopedica mexicana. 2020;34(6):441-9. DOI: 10.35366/99145.
- Gonçalves de Carvalho BK, Penha PJ, Ramos NLJP, Andrade RM, Ribeiro AP, João SMA. Age, sex, body mass index, and laterality in the foot posture of adolescents: A cross sectional study. J Manipulative Physiol Ther. 2020;43(7):744-52. DOI: 10.1016/j.jmpt.2018.11.035.
- Livingston LA, Mandigo JL. Bilateral rearfoot asymmetry and anterior knee pain syndrome. J Orthop Sports Phys Ther. 2003;33(1):4855.
- Nguyen AD, Shultz SJ. Sex differences in clinical measures of lower extremity alignment. J Orthop Sports Phys Ther. 2007;37(7):389-98. DOI: 10.2519/jospt.2007.2487.
- Ciufo DJ, Baker EA, Gehrke CK, Vaupel ZM, Fortin PT. Tibial torsion correlates with talar morphology. Foot Ankle Surg. 2022;28(3):354-61. DOI: 10.1016/j.fas.2021.04.007.
- Lafuente G, Munuera PV, Dominguez G, Reina M, Lafuente B. Hallux limitus and its relationship with the internal rotational pattern of the lower limb. J Am Podiatr Med Assoc. 2011;101(6):467-74. di:10.7547/1010467 DOI: 10.7547/1010467.
- Zhao X, Tsujimoto T, Kim B, Katayama Y, Tanaka K. Characteristics of foot morphology and their relationship to gender, age, body mass index and bilateral asymmetry in Japanese adults. J Back Musculoskelet Rehabil. 2017;30(3):527-35. DOI: 10.3233/BMR-150501.
- Verch R, Hirschmüller A, Müller J, Baur H, Mayer F, Müller S. Is in-toing gait physiological in children? - Results of a large cohort study in 5910 healthy (pre-) school children. Gait Posture. 2018;66:70-75. DOI: 10.1016/j.gaitpost.2018.08.019.
- Tong JW, Kong PW. Reliability of footprint geometric and plantar loading measurements in children using the Emed(®) M system. Gait Posture. 2013;38(2):281-86. DOI: 10.1016/j.gaitpost.2012.11.025.
- Katz K, Naor N, Merlob P, Wielunsky E. Rotational deformities of the tibia and foot in preterm infants. J Pediatr Orthop. 1990;10(4):483-85. DOI: 10.1097/01241398-199010040-00010.
- Furdon SA, Donlon CR. Examination of the newborn foot: positional and structural abnormalities. Adv Neonatal Care. 2002;2(5):248-58.