10.20986/revesppod.2025.1729/2025
CLINICAL CASE
Epidermoid carcinoma associated to onichocryptosis: a case report
Carcinoma epidermoide asociado a onicocriptosis: caso clínico
Antonio Javier González Fernández1
Lucía Trincado Villa1, Javier Pascual Huerta1
Alicia Gavillero Martín2
1Clínica del Pie Elcano. Bilbao, España.
2Departamento de Podología General Universidad Católica de Valencia “San Vicente Mártir”. Valencia, España
Abstract
Primary malignant tumors located in the nail or subungual area are rare, with squamous cell carcinoma or squamous cell carcinoma being the most common of all of them. The present work describes the progression of a clinical case of a patient with initial diagnosis of onychocryptosis, with a torpid evolution of the lesion and who after various conservative and surgical treatments ended with a diagnosis of squamous cell carcinoma and complete amputation of the first finger. The article shows the entire progression of the clinical picture from its beginning, emphasizing the importance of a high index of suspicion on the part of the clinician and the need for diagnosis through pathological anatomy in the event of an abnormal evolution of the lesion.
Keywords: Foot, nail, onychocrytosis, epidermoid carcinoma, squamous carcinoma, Winograd, amputation
Resumen
Los tumores malignos primarios de localización ungueal o subungueal son poco frecuentes, y el carcinoma epidermoide o carcinoma escamoso es el más común de todos ellos. El presente trabajo describe la progresión de un caso clínico de una paciente con diagnóstico inicial de onicocriptosis, con una evolución tórpida de la lesión la cual, tras diversos tratamientos conservadores y quirúrgicos, acabó con un diagnóstico de carcinoma epidermoide y amputación completa del primer dedo. En el artículo, se muestra toda la progresión del cuadro clínico desde su comienzo, enfatizando en la importancia de un alto índice de sospecha por parte del clínico y de la necesidad del diagnóstico mediante anatomía patológica ante una evolución anormal de la lesión.
Palabras clave: Pie, uña, onicocriptosis, carcinoma epidermoide, carcinoma escamoso, Winograd, amputación
Correspondence
Antonio Javier González Fernández
antgonfer94@gmail.com
Received: 09-03-2025
Accepted: 02-05-2025
Introduction
Primary malignant tumors of subungual localization are rare. Of these, squamous cell carcinoma (SCC) is the most prevalent in the foot(1,2). The most affected patients are between 50 and 60 years old, affecting men more than women, in a ratio of 3:12. The most common presentation is in the proximal and lateral nail folds and hyponychium and is characterized by erythema, paronychia, ulceration, hyperkeratosis, verrucous papules and plaques, subungual mass, onycholysis, and suppuration. These non-specific clinical characteristics mean that it can be easily confused with benign inflammatory processes such as paronychia, pyogenic granuloma, or a common wart, which often delays its initial diagnosis. When it affects the nail matrix, it can present with longitudinal erythronychia, melanonychia, and nail destruction(3). The diagnosis of these types of lesions is only possible through a biopsy and subsequent histopathological study. Treatment of these tumors involves complete excision, which sometimes means amputation of the distal phalanx of the affected toe(1,3,4,5,6,7).
This article illustrates the case report of a patient with a past medical history of onychocryptosis in the first toe of the foot with a torpid progression over time despite conservative and surgical treatment with several interventions, whose final diagnosis was squamous cell carcinoma. The objective is to present these types of cases to the podiatric community, highlighting the importance of performing a histopathological study in suspected cases or in those where the lesion evolves abnormally with conventional treatment. The article has been prepared following the CARE (CAse REport Statement) guidelines for the reporting and development of clinical cases in scientific journals(8).
Case report
A 50-year-old woman presented with a several-month history of pain and deformity in the first toe of her left foot in the context of several previous interventions on the first toe for medial border onychocryptosis. Relevant medical history includes no known drug allergies, smoker of 30 cigarettes/day, hypercholesterolemia, chronic diarrhea due to collagenous colitis, endometriosis, and depressive syndrome under psychiatric follow-up. Currently on treatment with: budesonide 3 mg (2-0-0), escitalopram 20 mg (1-0-0) and lormetazepam 2 mg (0-0-1), medroxyprogesterone 5 mg (1-0-0), calcium/vitamin D 1.5 g/400 IU (1-0-0), progesterone 100 mg (2-2-0).
The patient reported a 7-month history onychocryptosis (September 2022) on the medial border of the first toe of the left foot, with presence of ungual granulation tissue on said border, causing her pain and digital inflammation (Figure 1). The patient received treatment from her podiatrist consisting of chiropody and canal cleaning, and then daily dressings with mupirocin were prescribed for the lesion. The lesion showed poor progression in the following days with increased pain and tenderness to the touch. Treatment was modified to amoxicilin/clavulanic acid 875/125 mg, 1/8 hours along with the use of oral analgesics (Figure 2). The patient continued with poor symptomatic evolution and attended her health center where an X-ray was performed, ruling out the presence of deep infection (osteomyelitis).

Figure 1. Initial process of onicochryptosis and reactive granuloma.
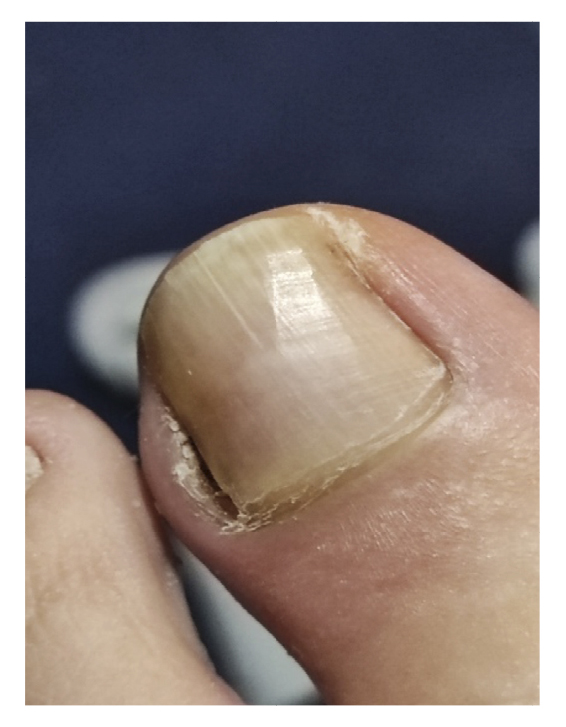
Figure 2. Clinical progressión after antibiotic and analgesic treatment.
After worsening of the clinical picture, on November 14th, 2022, a partial removal of the lateral nail plate of the left foot was performed at her health center along with curettage, removing hyperkeratotic and granulation tissue. The procedure was repeated 48 hours later (November 16th, 2022) because not all the lesion had been removed (Figure 3), changing the antibiotic treatment to anaclosil 500 mg 1/6 hours and then to ciprofloxacin 500 mg 1/12 hours during the following weeks.
The patient initially showed improvement in pain, although it never completely subsided (Figure 4). She reported recurrence of the nail lesion, which led her to seek a second opinion 6 weeks after the intervention with another podiatrist. This latter podiatrist, on December 27th (Figure 5), performed a bacterial culture of the lesion, which turned out negative, and also evaluated the lesion by ultrasound (without report). On January 13th, the patient underwent surgery using the phenol-alcohol technique on the lateral border of the first toe of the left foot (Figure 6).

Figure 3. 8th week. Partial resection of hyperplasic tissue performed in her medical center.

Figure 4. 9th-14th weeks. Recurrence of the lesión after partial resection.

Figure 5. 16th week. Negative microbiological culture and sonograhpic assessment (not available).
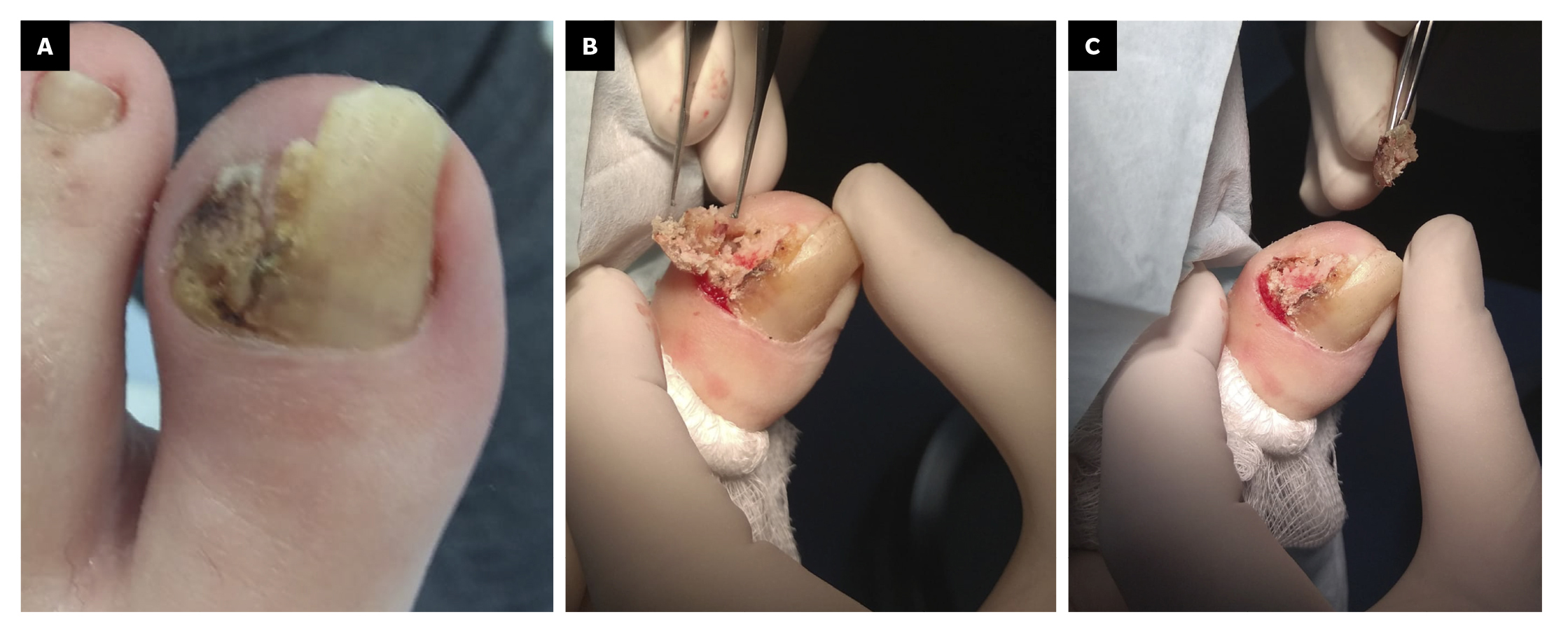
Figure 6. 18th week. Second intervention by means of phenol-alcohol partial matricectomy.
Within 3 weeks after the third intervention, the patient reported recurrence of the lesion and painful symptoms (Figure 7). The patient decided to attend the traumatology department (February 2023) where an MRI (T2FS and DPFATSAT) was requested. It showed an occupying mass in the lateral third of the first toe with well-defined borders and bone involvement (Figure 8) with the following report: “At the level of the distal phalanx of the 1st toe in the nail region, there appears to be a solution of skin continuity with a heterogeneous, a dense 15 mm x 14 mm collection in the lateral region of the parapharyngeal soft tissues, remodeling the bone and coming into contact with the flexor tendon, which could be consistent with a postoperative abscess/phlegmonous collection. Some bone edema in the distal phalanx is suspected, without completely ruling out incipient osteomyelitis. To be correlated with medical history and surgical protocol performed.”

Figure 7. 21th week. Recurrence of lesion after phenol-alcohol surgery.
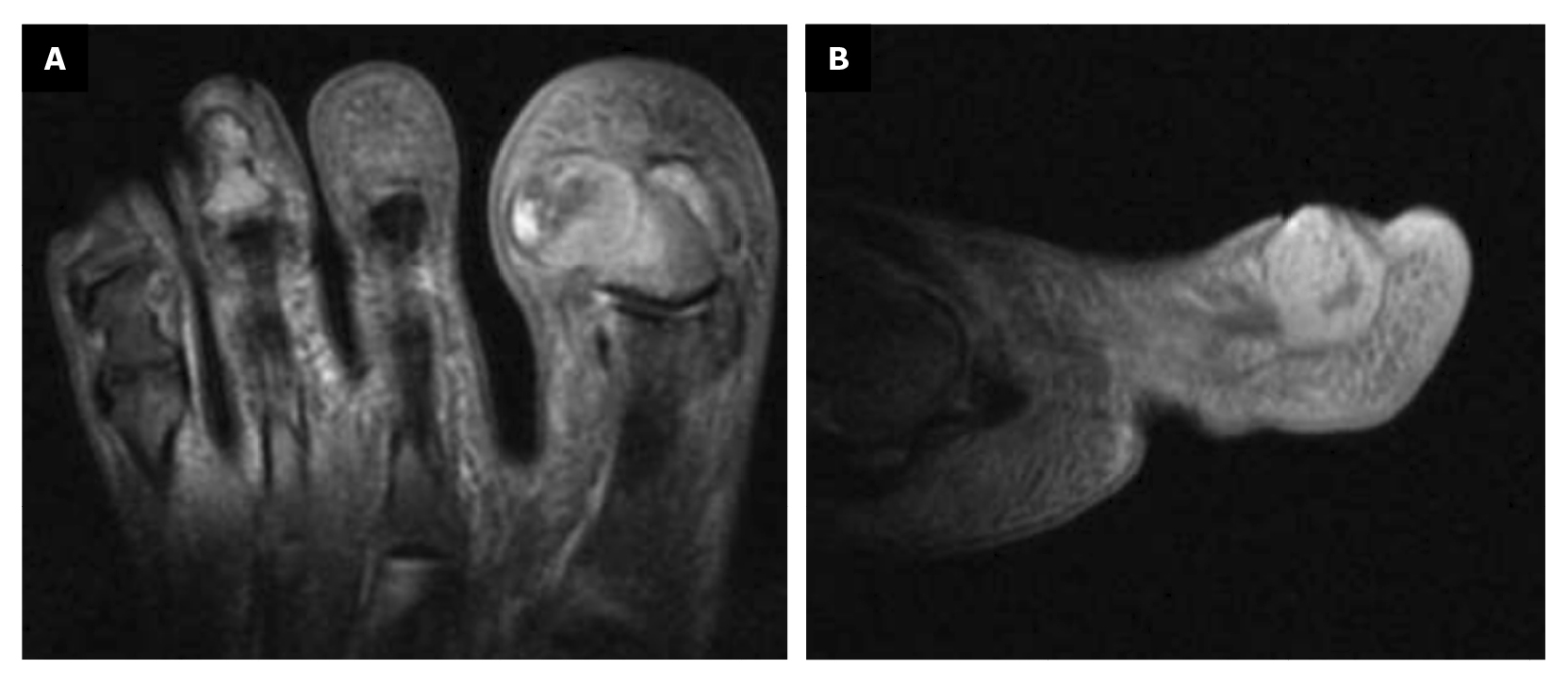
Figure 8. Space ocuping mass with bone involvement. A: transverse plane; B: saggital plane.
The Traumatology Service referred the patient to us, and she attended our center on February 27th, 2023. On March 1st, 2023, we decided to perform surgery with excisional biopsy of the lesion, with 5 mm safety margins around its contour. The lesion was completely removed, and given the bone involvement of the lesion, partial resection of the lateral border of the distal phalanx of the 1st toe was performed. Both samples (soft tissue and bone) were sent to pathology separately. Finally, the incision was closed with approximation sutures (Nylon 4/0) in the proximal and distal areas; since the primary defect was too large, the central area of the incision was left open to close by secondary intention with the use of hydrofiber (Figure 9).

Figure 9. A: 26th week; clinical aspect of the lesion; B-F: secuence of tumor excision with security margins and partial resection of distal phalanx.

Figure 10. 30th week with digital amputation.
The histopathological study of the samples described for the first sample: “Skin with a hyperkeratotic tumor composed of squamous cells with discrete atypia forming an expansive border with some cords and nests infiltrating the dermis. Lateral surgical margins free and deep margin affected. DIAGNOSIS: Well-differentiated infiltrating squamous cell carcinoma affecting the deep margin,” and for the second sample: “Bone tissue with bone trabeculae and adipose tissue between them without alterations. Focally, two small nests of well-differentiated squamous cell carcinoma are observed. DIAGNOSIS: Bone tissue with focal infiltration by well-differentiated squamous cell carcinoma.”
5 days postoperatively, the patient’s first dressing change was performed, which showed a good appearance and no local infection. The patient was explained the result of pathology and referred to the oncology service of her hospital, and from there to the dermatology and plastic surgery service where digital amputation was performed (Figure 10). Subsequent follow-up was conducted by the Oncology service for the next 6 months. After different tests, it was determined that no other treatment was needed. Figure 11 shows the timeline of the clinical case.
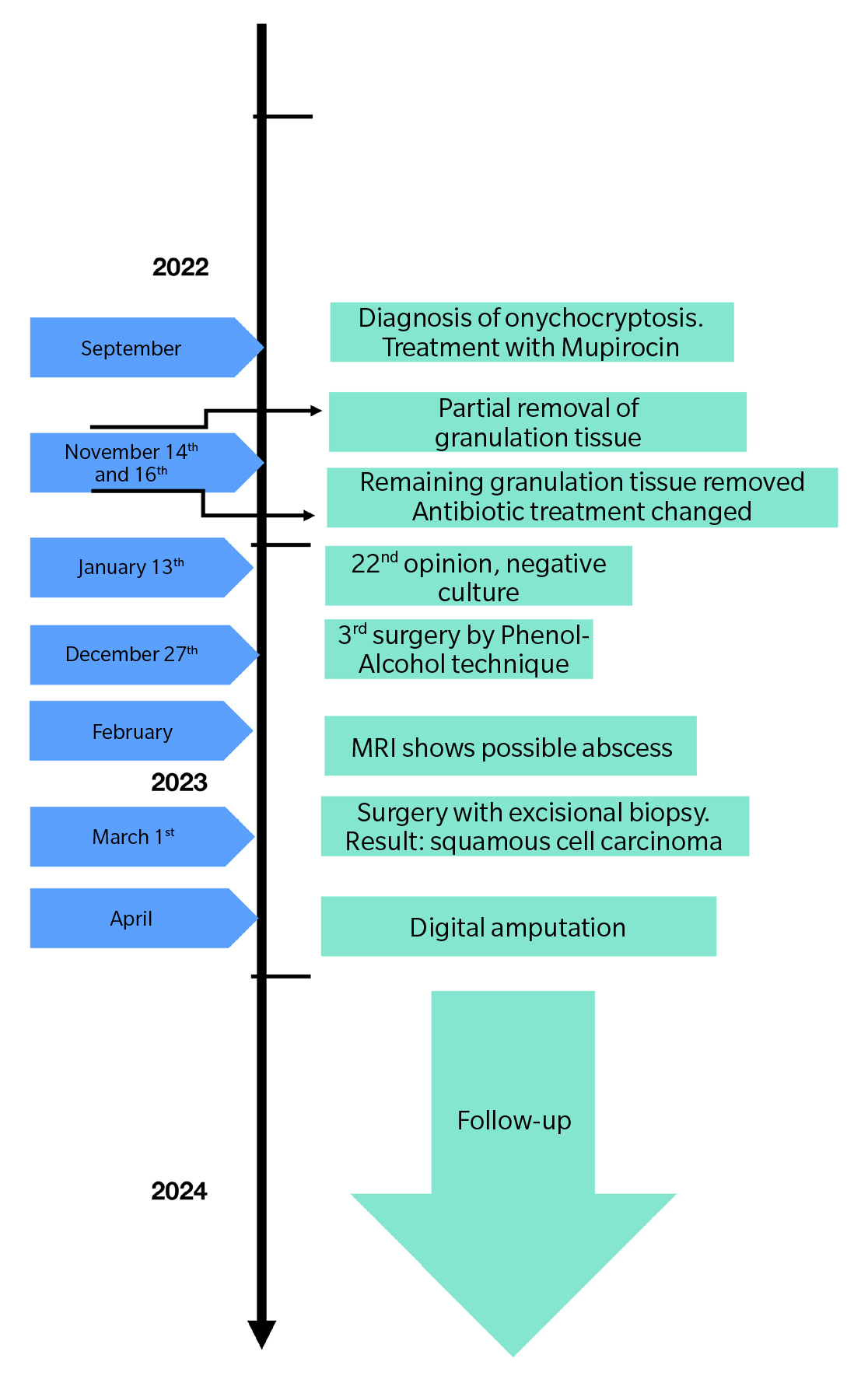
Figure 11. Case timeline.
Discussion
This article presents an atypical case of onychocryptosis, which ultimately led to a diagnosis of squamous cell carcinoma and resulted in complete amputation of the first toe. The objective is to introduce this pathology, although rare, to the podiatric community. Subungual squamous cell carcinoma (SCC) was first described by Velpeau in 1850. It is a neoplasm with low aggressive potential. It has a tendency to affect bone (described in up to 66% of cases) as in the case we presented. However, it rarely metastasizes(1,2).It frequently presents in men between 50 and 70 years old. Although it is more common in fingers, it can also occur in toes(4).. Up to 75% of cases are associated with human papillomavirus, especially serotypes 16, 18, 35, 56. In the feet, risk factors are thought to be: ulcers, chronic granulomas, trauma and chronic inflammation, exposure to tobacco smoke or solar radiation(2,3,4,5).
The clinical presentation depends on the location of the pathological process within the nail unit. When it affects the proximal or lateral nail fold or the hyponychium, it can present as erythema, verrucous papules, onycholysis, or suppuration. If it affects the nail matrix, it presents with longitudinal erythronychia and frequently nail destruction. If it affects the nail bed, it can present with onycholysis and suppuration, along with red papules and nodules(2,3).
It is a progressive and invasive tumor, typically presenting with a delay in diagnosis of years(1,2). The lesions can be painful. Given that the clinical presentation is similar to other benign nail conditions such as paronychia, wart, onychomycosis, nail dystrophy, pyogenic granuloma, onychocryptosis, and onycholysis with infection, a high index of suspicion must be maintained, and all these conditions that do not respond to the prescribed therapy should be biopsied(2,3,4,5,6,7).This is the case in the article we present, in which the patient’s condition showed an abnormally strange evolution that did not correspond to the natural history of the disease. Maintaining a high index of suspicion along with histopathological analysis is key in this type of condition with atypical evolution. If the lesion is located in the nail fold, a wide longitudinal biopsy is preferable. Dermoscopy is a tool that can aid in the diagnosis of these lesions(2,3).Finally, imaging tests such as plain radiography or MRI are necessary to assess bone involvement(2,4).
The treatment of choice is surgery, preferably Mohs surgery to excise the tumor with a complete margin analysis, and subsequent skin defect coverage(4,7).In the present case, surgery was performed to remove the entire tumor, respecting 5 mm safety margins around the lesion and performing excision of the lateral border of the distal phalanx (in direct contact with the tumor) with the aim of trying to save the distal phalanx of the first toe. The samples sent separately for histopathology showed the presence of involvement in the distal phalanx that had not been entirely removed. In invasive lesions with bone involvement, it is recommended to excise the entire nail unit along with disarticulation of the toe and amputation of the phalanx(2,3,4,5,6)..
In conclusion, squamous cell carcinoma, although a rare entity, should be considered, as its non-specific presentation delays its diagnosis and treatment, thereby requiring more radical procedures with more compromised functional outcomes for our patients. Early biopsy and histopathological study are key to enabling early diagnosis, improving our patients’ prognosis and sequelae.
Authors’ contribution
Creation, writing, and draft preparation: AJGF, LTV, JPH, AGM. Final review: AJGF, LTV, JPH, AGM.
Ethical statement
The patient in the clinical case has given her explicit consent for the realization of this article, providing all the graphical documentation of the case she had, observing the follow-up of the entire process.
Funding
None declared.
Conflicts of interest
None declared.
References
- Gómez Vázquez M, Navarra Amayuelas R, Martin-Urda MT, Abellaneda Fernández C, Tapia G. Subungual squamous cell carcinoma. Presentation of two cases. Actas Dermosifiliogr. 2010;101(7):654-56. DOI: 10.1016/j.ad.2010.02.009.
- Knackfuss IG, Giordano V, Godoy-Santos AL, Fernandes NC, Camargo OP. Squamous cell carcinoma in the foot: Case series and literature review. Acta Ortop Bras. 2018;26(2):108-11. DOI: 10.1590/1413-785220182602187183.
- Hare AQ, Rich P. Nail tumors. Dermatol Clin. 2021;39(2):281-92. DOI: 10.1016/j.det.2020.12.007.
- Dijksterhuis A, Friedeman E, van der Heijden B. Squamous cell carcinoma of the nail unit: Review of the literature. J Hand Surg Am. 2018;43(4):374-9.e2. DOI: 10.1016/j.jhsa.2018.01.010.
- Padilha CB, Balassiano LK, Pinto JC, Souza FC, Kac BK, Treu CM. Subungual squamous cell carcinoma. An Bras Dermatol. 2016;91(6):817-9. DOI: 10.1590/abd1806-4841.20165084.
- Wong KY, Ching DL, Gateley D. Subungual squamous cell carcinoma. BMJ Case Rep. 2015;2015:bcr2014207565. DOI: 10.1136/bcr-2014-207565. DOI: 10.1136/bcr-2014-207565.
- García-Zamora E, Miñano Medrano R, Vicente-Martín FJ, Pinedo Moraleda F, García-García E, López-Estebaranz JL. Mohs micrographic surgery in squamous cell carcinoma of the nail unit Actas Dermosifiliogr. 2022;113:T526-8. DOI: 10.1016/j.ad.2020.08.039.
- Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; CARE Group. The CARE guidelines: Consensus-based clinical case reporting guideline development. Glob Adv Health Med. 2013;2(5):38-43. DOI: 10.7453/gahmj.2013.008.